Taking medication should make you feel better, not worse. But sometimes, what starts as a simple side effect can turn into something serious-fast. If you’re on prescription drugs or even over-the-counter pills, knowing when to call your doctor isn’t just helpful; it can save your life.
What Counts as a Red Flag?
Not every weird feeling means something’s wrong. Nausea after antibiotics? Common. Dry mouth from antihistamines? Normal. But some symptoms aren’t just uncomfortable-they’re warning signs. The FDA defines a serious reaction as one that causes death, hospitalization, disability, permanent damage, or a birth defect. That’s the line you need to know.Here’s what you should never ignore:
- Difficulty breathing-even if it’s just a little tightness in your chest or throat. This is the #1 sign of anaphylaxis, a life-threatening allergic reaction that can hit within minutes.
- Hives or swelling-especially on your face, lips, tongue, or throat. If you notice red, raised bumps or your lips suddenly look puffy, don’t wait.
- Blisters or peeling skin-this could be Stevens-Johnson Syndrome (SJS) or toxic epidermal necrolysis (TEN). These rare but deadly reactions often start with flu-like symptoms, then turn into painful blisters that spread. About 100-200 cases are reported in the U.S. each year, and they need hospital care immediately.
- Fainting or feeling like you’re about to-dizziness is one thing; passing out is another. A sudden drop in blood pressure can signal a severe reaction to blood pressure meds, antibiotics, or even heart drugs.
- Severe nosebleeds or unexplained bruising-if you’re on blood thinners like warfarin or apixaban, minor bleeding is expected. But if you’re bleeding for more than 10 minutes or bruising without bumping into anything, call your doctor.
- Confusion, slurred speech, or weakness on one side-this could point to a stroke caused by a drug interaction or bleeding in the brain.
These aren’t "maybe" situations. If you have even one of these, call emergency services or go to the ER. Don’t text your doctor. Don’t wait until morning. Time matters.
When Is It Just a Side Effect?
Most side effects aren’t dangerous. In fact, they’re common. About 20-30% of people on antibiotics feel nauseous. Half of opioid users get constipated. One in three people on antihistamines feel drowsy. These aren’t reasons to quit your medicine.The National Institutes of Health says stopping medication without talking to your provider is one of the biggest reasons treatment fails. For chronic conditions like high blood pressure, diabetes, or depression, 40% of complications happen because people quit their meds too soon.
So how do you tell the difference?
- Minor side effects: Mild nausea, dry mouth, drowsiness, headache, mild rash, diarrhea. These usually fade after a few days as your body adjusts.
- When to worry: If it gets worse after 72 hours. If it stops you from sleeping, eating, or working. If it’s new and intense, especially if you just started a new drug.
Harvard Health Publishing says: If a side effect bothers you for more than 48 hours-or if it cuts into your daily life by more than 30%-it’s time to call. Not panic. Just call.
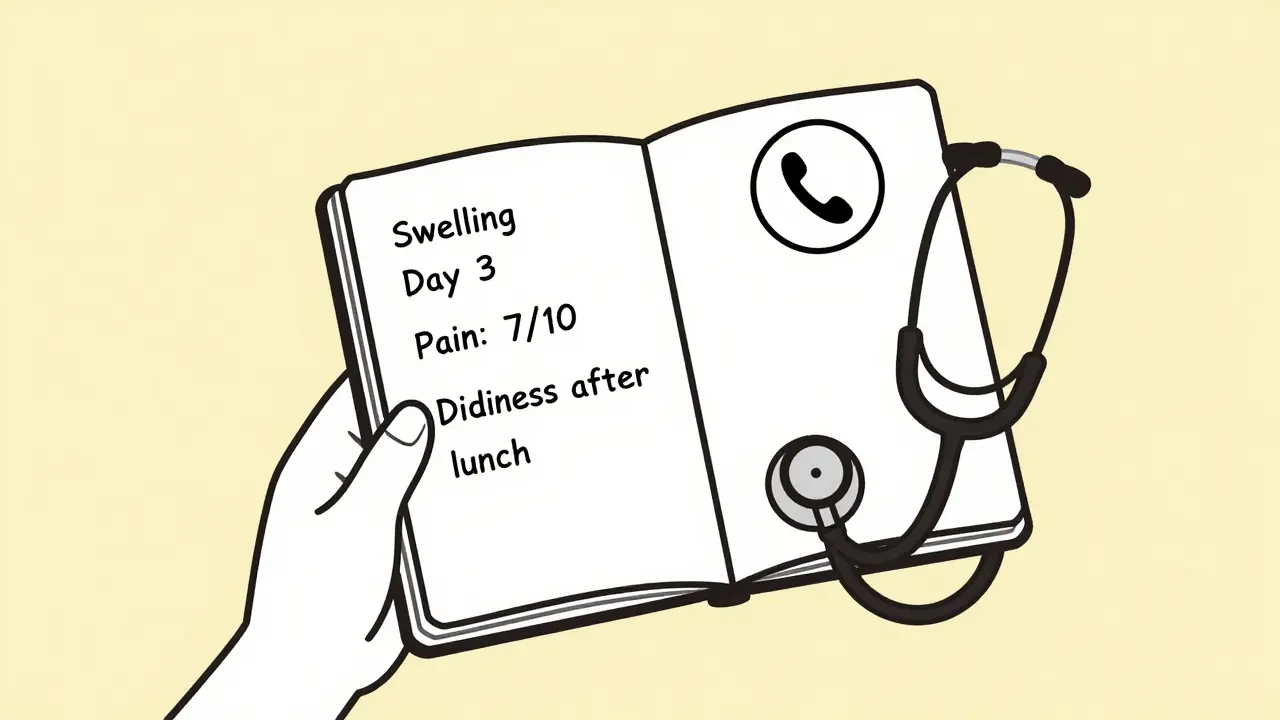
Keep a Side Effect Diary
You’d be surprised how much detail helps your doctor. A 2022 Lancet study found that patients who kept a side effect diary improved diagnostic accuracy by 65%. That’s huge.Here’s how to do it:
- Write down the symptom: "Swelling in my ankles," not just "my legs hurt."
- When did it start? "Three days after I started the new blood pressure pill."
- How bad is it? Rate it 1-10. "Pain is a 7, constant."
- What time of day? "Dizziness hits right after lunch, every day."
- Did anything help? "Sat down, drank water, felt better in 15 minutes."
Bring this to your next appointment-or send a photo of it to your doctor’s portal. This isn’t extra work. It’s your best tool for getting the right answer fast.
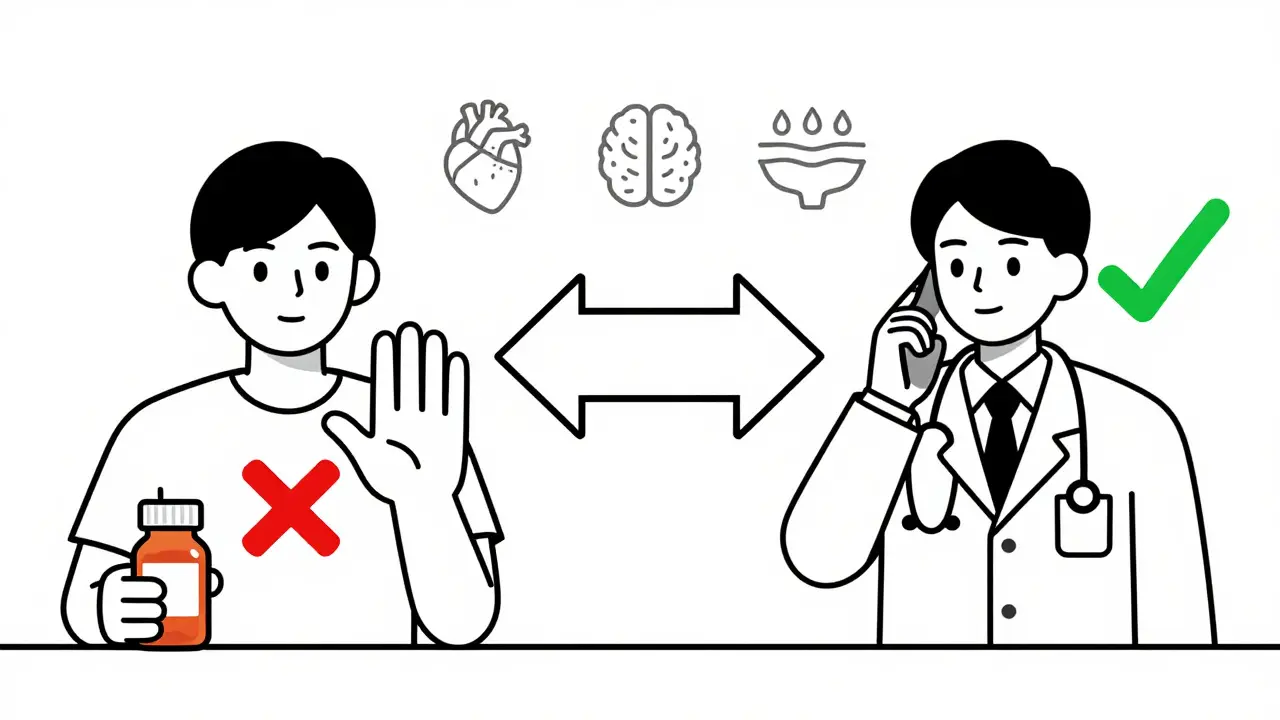
Don’t Stop Your Meds (Unless It’s an Emergency)
A lot of people panic when they feel off and quit their meds. That’s dangerous.For example, if you’re on a beta-blocker for heart issues and you feel dizzy, stopping it cold turkey can cause your heart rate to spike, triggering a heart attack. If you’re on antidepressants and quit suddenly, you can get withdrawal seizures. Even for antibiotics, stopping early can lead to resistant infections.
The rule? Only stop if you have signs of anaphylaxis or severe skin reactions. That means trouble breathing, swelling of the throat, or blisters covering more than 10% of your skin. Everything else? Call your doctor. They might adjust the dose, switch the drug, or add something to help with the side effect.
As Dr. Robert Wood from Johns Hopkins says: "Anaphylaxis can kill in minutes. Everything else? We can fix it."
How to Report a Bad Reaction
Your report matters. The FDA’s MedWatch program gets over 1.3 million adverse event reports every year. About 15-20% come from patients like you. These reports have led to 200-300 label changes and 15-20 drug recalls since 2020.Reporting is easy:
- Call 1-800-332-1088 (toll-free in the U.S.)
- Or go to fda.gov/medwatch (you can still report even if you’re outside the U.S.)
You don’t need a diagnosis. Just say: "I took this drug and had this reaction." Include the drug name, dose, when you took it, and what happened. The FDA uses this data to update warnings, change packaging, or pull dangerous drugs off the market.
It’s not just about you. It’s about the next person who might take that same pill.
What’s Changing in Medication Safety
The FDA just started a big push to make side effect info clearer. Starting January 1, 2025, all new medication guides must use plain language-not medical jargon. Instead of "gastrointestinal disturbance," you’ll see "stomach upset or diarrhea."The Sentinel Initiative, which tracks health data from 300 million patients, has already caught dangerous drug patterns faster than ever. In 2022, it spotted a heart failure risk with a diabetes drug within six months-something that used to take years. That’s saved lives.
And it’s not just tech. Pharmacies now hand out medication guides for 92% of high-risk drugs. The National Library of Medicine’s DailyMed database gives free, up-to-date side effect info for over 140,000 medications. Use it. Search your drug name. Read what’s listed.
Final Advice: Be Your Own Advocate
You know your body better than anyone. If something feels off, it probably is. Don’t second-guess yourself because "it might just be a side effect." And don’t wait for someone else to notice.Keep your meds list updated. Tell your doctor about every supplement, OTC pill, and herbal tea you take. Many dangerous interactions happen because no one knew you were taking ginger capsules with your blood thinner.
And remember: calling your doctor isn’t a burden. It’s part of staying healthy. Most doctors prefer you call with a question than show up in the ER because you waited too long.
What should I do if I think I’m having an allergic reaction to my medication?
If you have trouble breathing, swelling of your face or throat, hives, or feel like you’re going to pass out, call emergency services immediately. Do not wait. If you have an epinephrine auto-injector (like an EpiPen), use it right away. Even if symptoms seem to fade, you still need to go to the hospital-reactions can come back.
Can I stop taking my medication if side effects are annoying but not dangerous?
No-not without talking to your doctor first. Stopping meds like those for blood pressure, diabetes, seizures, or depression can cause serious health problems, including heart attacks, seizures, or relapses. Many side effects fade after a few days or can be managed with dose changes or added medications. Always ask before quitting.
How long should I wait before calling my doctor about a side effect?
If a side effect lasts more than 48 hours, gets worse, or interferes with your daily life (like making it hard to sleep, work, or eat), call your doctor. Don’t wait until it’s unbearable. Early action can prevent complications and help you stay on the right treatment.
Are over-the-counter drugs safe to take with prescription meds?
Not always. Common OTC drugs like ibuprofen, antacids, or cold medicines can interact with blood thinners, antidepressants, or heart medications. For example, mixing ibuprofen with warfarin increases bleeding risk. Always check with your pharmacist or doctor before adding any new pill-even if it’s "natural" or sold without a prescription.
What if I don’t have a doctor or can’t afford to see one?
In New Zealand, you can call Healthline (0800 611 116) for free, 24/7 advice from trained nurses. They can help you decide if your symptoms need urgent care or if you can wait. Many clinics also offer low-cost or sliding-scale visits. Your safety matters more than cost. Don’t delay help because you’re worried about the bill.
