When your kidneys aren’t working well, what you eat becomes just as important as any medication. A renal diet isn’t about losing weight or eating ‘clean’-it’s about protecting what’s left of your kidney function and avoiding dangerous buildups in your blood. Too much sodium, potassium, or phosphorus can lead to swelling, heart problems, bone damage, or even sudden cardiac arrest. The good news? With the right knowledge, you can eat well, feel better, and slow down kidney damage.
Why Sodium Matters in Kidney Disease
Your kidneys help balance sodium in your body. When they’re weak, sodium builds up, pulling water with it. That means swelling in your ankles, shortness of breath from fluid in your lungs, and high blood pressure that strains your heart and kidneys even more. The standard advice? Keep sodium under 2,000 to 2,300 milligrams a day. That’s about one teaspoon of salt. But here’s the catch: most sodium doesn’t come from the salt shaker. It comes from packaged and processed foods. A single can of soup can have 800-1,200 mg. One slice of processed cheese? Around 400 mg. Bread, deli meats, frozen meals, and even some breakfast cereals are loaded. Reading labels is non-negotiable. Look for “low sodium,” “no salt added,” or “unsalted.” Avoid anything with more than 140 mg per serving. Swap out salty snacks for fresh fruit, unsalted popcorn, or rice cakes. Use herbs like oregano, thyme, or garlic powder instead of salt. The CDC found that cutting just 1,000 mg of sodium daily can lower systolic blood pressure by 5-6 mmHg-big for your heart and kidneys.Potassium: The Silent Threat
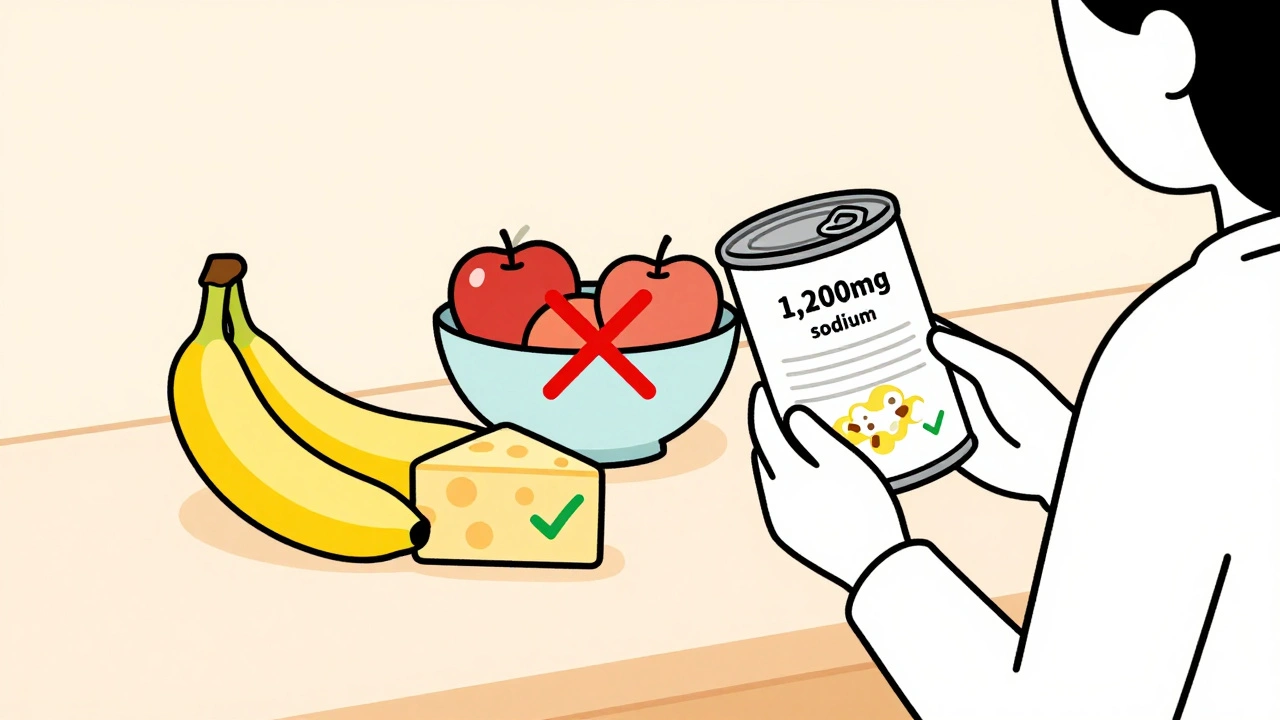
Potassium helps your muscles and heart work right. But when your kidneys can’t remove it, levels rise. Above 5.5 mEq/L, you risk irregular heartbeat-or worse. For most people with stage 3-5 chronic kidney disease, the goal is 2,000-3,000 mg per day. But this isn’t one-size-fits-all. Your doctor will adjust based on your blood tests. High-potassium foods are often called “healthy”-bananas, oranges, potatoes, tomatoes, spinach, and avocados. These need to be limited or swapped. A medium banana has 422 mg. A cup of cooked spinach? 840 mg. That’s more than your daily limit in one serving. Better choices? Apples (150 mg each), berries (65 mg per ½ cup blueberries), cabbage (12 mg per ½ cup cooked), and green beans. Even better? Leach high-potassium veggies like potatoes or carrots. Peel them, slice thin, soak in warm water for 2-4 hours, then boil in plenty of water. This cuts potassium by nearly half. Also, remember this: potassium from animal foods (meat, dairy) is absorbed more easily than from plants. So if your levels are high, you may need to cut back on milk, yogurt, and even lean meats-even if they’re low in sodium.Phosphorus: The Hidden Problem
Phosphorus helps build bones and store energy. But when your kidneys fail, it builds up. High phosphorus pulls calcium out of your bones, making them weak and brittle. It also causes dangerous calcifications in your blood vessels and heart. The target? 800-1,000 mg per day for non-dialysis patients. But here’s what most people don’t know: not all phosphorus is the same. Natural phosphorus in foods like meat, dairy, nuts, and beans is only 40-70% absorbed. But added phosphorus in processed foods? Almost 100% absorbed. That’s why colas, processed cheese, deli meats, and instant mashed potatoes are worse than steak or milk. A 12-ounce cola has 450 mg. One slice of processed cheese? 250 mg. A cup of milk? 125 mg. So you can have milk in small amounts-but avoid soda and cheese slices. White bread is safer than whole grain (60 mg vs. 150 mg per slice). Rice and pasta are better than bran cereals. Choose fresh meats over processed ones. And if you’re on dialysis, your doctor may prescribe phosphate binders-meds you take with meals to block absorption.Protein: The Balance Game
You’ve probably heard to eat less protein with kidney disease. That’s true-but not as much as you think. Too little protein leads to muscle loss, weakness, and higher risk of infection. Too much? It overwhelms your kidneys. The current sweet spot? 0.55 to 0.8 grams of protein per kilogram of body weight. For a 70 kg (154 lb) person, that’s 38-56 grams a day. Focus on high-quality protein: eggs, fish, chicken, and lean cuts of meat. A 3-ounce portion of salmon, cod, or tuna has about 20-25 grams of protein and is low in sodium. Eat it two to three times a week. Avoid plant proteins like tofu and legumes if your phosphorus or potassium is high. They’re harder to manage. But if your labs are stable, small portions of lentils or chickpeas can be included.Real-Life Swaps That Work
Changing your diet doesn’t mean giving up flavor or satisfaction. It means smarter choices.- Instead of potato chips: try air-popped popcorn with a sprinkle of paprika
- Instead of orange juice: drink apple or cranberry juice (check labels for added potassium)
- Instead of white rice: try white pasta or refined grains (lower in phosphorus than brown rice)
- Instead of canned vegetables: use fresh or frozen (rinse canned veggies well to reduce sodium)
- Instead of salted butter: use olive oil or herb-infused oils
Fluids, Supplements, and New Tools
If you’re making little or no urine, you’ll also need to limit fluids. Most people are told to stick to 32 ounces (about 1 liter) a day. That includes water, coffee, tea, soup, ice cream-even ice cubes. Medicare now covers up to six sessions a year with a renal dietitian for stage 4 CKD patients. That’s because personalized advice saves money-and lives. One study found that proper diet management delays dialysis by 6-12 months, saving $12,000 per person annually. New tools are helping. Apps like Kidney Kitchen let you scan barcodes and track sodium, potassium, and phosphorus in real time. The FDA even approved Keto-1 in 2023-a medical food designed to provide essential nutrients while keeping phosphorus and potassium low. Emerging research is looking at gut health. Prebiotic fibers like inulin may reduce phosphorus absorption by 15-20%. The NIH’s PRIORITY study is testing genetic tests to predict how your body handles these minerals-so one day, your diet might be tailored to your DNA.
What Not to Do
Don’t assume “natural” means safe. Natural foods like bananas, potatoes, and dairy are high in potassium and phosphorus. Don’t take over-the-counter supplements without checking with your doctor. Many contain hidden potassium or phosphorus. Don’t quit the diet because it’s hard. The first 3-6 months are the toughest. Taste buds adjust. Meal planning gets easier. You’ll learn which foods you can have, how much, and how to prepare them. Don’t compare your plan to someone else’s. Your needs are based on your labs, stage of disease, and other conditions like diabetes. What works for your friend might be dangerous for you.When to Call Your Doctor
If you notice:- Swelling in your legs or face that doesn’t go away
- Heart palpitations or feeling lightheaded
- Extreme fatigue or muscle cramps
- Nausea, vomiting, or loss of appetite
Final Thought: It’s Not About Perfection
You don’t have to be flawless. Some days you’ll eat something off-plan. That’s okay. What matters is consistency over time. Every time you choose an apple over a banana, white rice over brown, or fresh chicken over deli meat-you’re giving your kidneys a break. The goal isn’t to live on a diet forever. It’s to live well with your kidneys for as long as possible. And with the right tools, support, and small daily choices-you absolutely can.Can I still eat fruits and vegetables on a renal diet?
Yes-but you need to pick carefully. Low-potassium options like apples, berries, cabbage, green beans, and cauliflower are safe in normal portions. High-potassium ones like bananas, oranges, potatoes, tomatoes, and spinach should be limited or leached (soaked and boiled) to reduce potassium. Portion size matters: a half-cup of cooked spinach is safer than a whole cup.
Is sea salt or Himalayan salt better than table salt?
No. All types of salt are made of sodium chloride. Whether it’s table salt, sea salt, or Himalayan salt, they all contain sodium. One teaspoon of any of them has about 2,300 mg of sodium-the full daily limit for most people with kidney disease. Avoid all added salt, regardless of type.
Can I drink milk on a renal diet?
In small amounts, yes. One half-cup of milk has about 125 mg of phosphorus and 150 mg of potassium. That’s acceptable if you’re keeping your daily totals low. But avoid large servings, and don’t drink it with every meal. Consider non-dairy alternatives like rice milk (check labels-some are fortified with phosphorus). Almond milk is often lower in phosphorus but watch for added potassium or phosphorus additives.
Why are processed foods so bad for a renal diet?
Processed foods contain added sodium, phosphorus, and sometimes potassium for flavor, texture, and shelf life. The phosphorus additives-like sodium phosphate or calcium phosphate-are almost 100% absorbed by your body, unlike natural phosphorus in meat or dairy. One soda or slice of processed cheese can give you half your daily phosphorus limit. Reading labels and choosing whole, unprocessed foods is the best defense.
Should I take vitamin or mineral supplements?
Only if prescribed by your doctor. Many over-the-counter vitamins, especially those labeled “for kidney health,” contain potassium, phosphorus, or other minerals that can be harmful. Even calcium supplements can raise phosphorus levels. Always check with your nephrologist or dietitian before taking anything.
How long does it take to adjust to a renal diet?
Most people need 3 to 6 months to get used to the changes. The first few weeks are the hardest-food can taste bland without salt, and planning meals feels overwhelming. But over time, your taste buds adapt. You’ll start to enjoy the natural flavors of food. Many people say they feel better, have less swelling, and sleep better within a few weeks of sticking to the plan.
Can a renal diet help me avoid dialysis?
Yes, for many people. Studies show that following a proper renal diet can delay the need for dialysis by 6 to 12 months, especially in stage 4 chronic kidney disease. It reduces the workload on your kidneys, controls blood pressure, and prevents dangerous mineral buildups. It’s not a cure, but it’s one of the most powerful tools you have to protect your kidneys.
Shannara Jenkins
Just started my renal diet last month and honestly? It’s been a game-changer. No more puffiness in my ankles, and my blood pressure is finally in range. Took me a week to stop missing salt, but now I love how herbs like garlic powder and oregano bring flavor without the danger. You don’t have to give up eating-you just have to eat smarter.
Jay Everett
Yessss!! 🙌 I used to think ‘healthy’ meant bananas and spinach-turns out those are kidney killers 😅 Leaching potatoes changed my life. I slice ‘em thin, soak ‘em overnight, boil ‘em like pasta… now I can enjoy mashed potatoes without feeling guilty. And yes, rice milk over almond milk-watch out for added phosphorus in the latter! Kidney Kitchen app is my BFF now.
Elizabeth Grace
I hate this diet so much. I miss cheese. I miss pizza. I miss salt. I cry when I see my mom eating a bag of chips and I can’t even have one bite. Why does my body have to do this to me? 😭
Alicia Marks
You’re not alone. It’s hard, but it gets easier. I cried too. Now I make my own ‘cheesy’ cauliflower bake with nutritional yeast. Tastes like comfort. You’ve got this.
Paul Keller
While the dietary recommendations are generally sound, they lack sufficient nuance regarding individual metabolic variability. The assumption that 2,000 mg of sodium is universally appropriate for all stage 3-5 CKD patients is clinically reductive. Some patients exhibit salt-resistant hypertension; others, particularly those with comorbid diabetes, require stricter limits. Furthermore, the article fails to address the confounding effects of diuretic use on electrolyte excretion-a critical oversight in clinical practice.
The assertion that phosphorus additives are ‘100% absorbed’ is an oversimplification. Bioavailability varies by food matrix and gastric pH, and recent studies suggest that phytate-rich foods may mitigate absorption even in processed items. Additionally, the recommendation to avoid plant proteins entirely is outdated; emerging data from the CRIC study indicates that controlled legume intake, paired with phosphate binders, may be safe and beneficial in select populations.
Moreover, the promotion of apps like Kidney Kitchen as definitive tools ignores their reliance on incomplete FDA food databases. Many proprietary formulations, especially in ethnic or artisanal products, are misclassified. A more rigorous approach would involve personalized lab-guided adjustments rather than generalized thresholds.
Finally, the notion that dietary adherence delays dialysis by 6–12 months is statistically misleading. The cited study had a small sample size and lacked control for medication compliance. Correlation does not imply causation. We must avoid therapeutic nihilism or false hope based on anecdotal extrapolation.
Laura Baur
Paul, your comment is not just overly technical-it’s dangerously misleading. You’re implying that people should ignore guidelines because ‘it’s complicated.’ That’s the exact mindset that gets patients to dialysis early. People need clear, actionable rules-not academic caveats. If someone’s reading this because they’re terrified of dying, they don’t need a lecture on bioavailability. They need to know: skip the soda, rinse the beans, avoid processed cheese. Period.
And for the record, the CRIC study you referenced didn’t support ‘controlled legume intake’ as a green light-it said ‘cautious inclusion under supervision.’ You’re twisting data to sound smart. That’s not expertise. That’s arrogance.
Also, ‘nutritional yeast’? Please. That’s not ‘cheesy.’ That’s fungus dust with a fancy name. Real cheese has flavor. Real food has taste. You’re not healing your kidneys-you’re just becoming a sad, bland robot.
dave nevogt
I’ve been on this diet for three years. The first six months felt like mourning. I missed the way food used to taste. But slowly, I started noticing things I hadn’t before-the sweetness in a ripe apple, the earthiness of boiled carrots, the way olive oil drizzled on steamed green beans feels like a gift. It’s not about restriction. It’s about recalibrating your relationship with food. You’re not losing flavor. You’re learning to hear it again.
And to Elizabeth-you’re not weak for crying. This diet steals more than salt. It steals memories. But your tears aren’t failure. They’re proof you care. And that’s the first step to healing.
Steve Enck
Let us not delude ourselves. The entire renal diet paradigm is a capitalist construct designed to prolong the life of patients while maximizing pharmaceutical revenue. Dialysis is a multi-billion-dollar industry. The ‘delay dialysis’ narrative serves institutional interests far more than it serves individual health. Why do you think Medicare now covers dietitians? Because it’s cheaper than hemodialysis. You are not being empowered-you are being managed.
The notion that ‘small daily choices’ matter is a psychological smokescreen. If your kidneys are failing, no amount of leached potatoes will restore nephron function. The real solution lies in organ transplantation or regenerative medicine-not in avoiding colas. We are treating symptoms while ignoring the disease.
And yet, I still follow the diet. Because I am not a philosopher. I am a survivor. And survival, in this system, means playing the game-even when you know the board is rigged.
Rebecca M.
Wow. So let me get this straight. I can’t have a banana, but I can have a soda? Wait-no, I can’t have soda either because of phosphorus. But I can have rice milk… unless it’s fortified. And I can eat chicken but not tofu? So what’s left? Air? Water? Sadness?
I mean, I get it. But it’s like being told you can’t hug anyone, but you can hug a pillow. And the pillow has a nutrition label.
Roger Leiton
😂😂😂 Rebecca, you just described my entire life. I’m currently eating a bowl of boiled white rice with a sprinkle of paprika and crying into it. My cat judges me. My dog just licked my plate. I think he’s trying to help.
Also-anyone else notice how the article never mentions how hard it is to find low-phosphorus snacks? I tried ‘low-sodium’ pretzels. Turned out they had calcium phosphate. I almost cried. Again.
Lynn Steiner
USA rules. We don’t need some fancy diet to tell us how to eat. Back in my day, we ate what we killed. No labels. No apps. No ‘phosphorus binders.’ If your kidneys fail, maybe you weren’t meant to live. Just sayin’.
Jack Dao
Let me be the first to say it: this post is a masterpiece of medical propaganda. The author is clearly a paid shill for the renal diet industrial complex. They mention ‘new tools’ like Keto-1 and the NIH’s PRIORITY study like they’re miracles. But where’s the independent research? Where’s the conflict-of-interest disclosure? Who funded this? Big Pharma? The kidney clinic chain?
And why does every single recommendation align perfectly with the products sold by the ‘Renal Nutrition’ brand? Coincidence? I think not.
Real healing comes from fasting, alkaline water, and avoiding all processed foods-including the ‘low-sodium’ ones. This is just another way to sell you pills and meal plans while pretending you’re in control.