Myxedema coma is not just a rare complication of hypothyroidism-it’s a ticking clock. Every hour without treatment increases the chance of death by 10%. This isn’t a slow decline. It’s a sudden, silent collapse of the body’s most vital systems, often hidden behind symptoms doctors mistake for old age, depression, or infection. And yet, it’s completely treatable-if you know what to look for and act fast.
What Exactly Is Myxedema Coma?
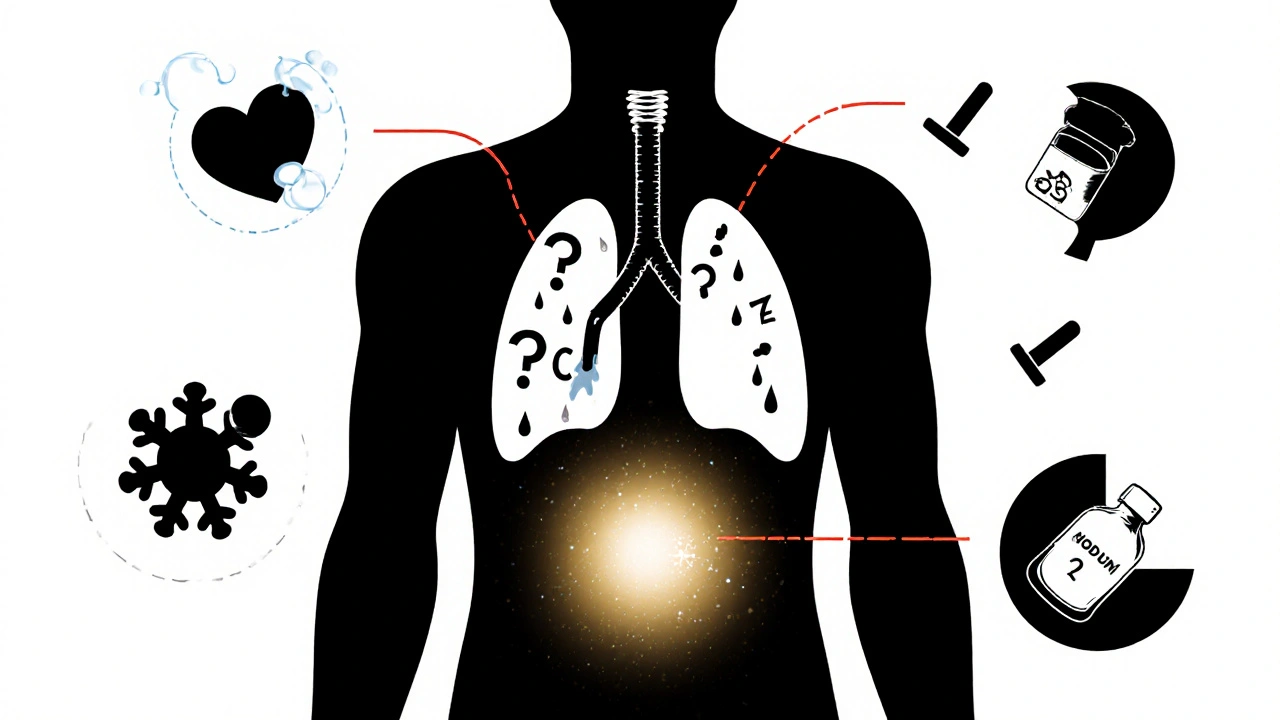
Myxedema coma, now more accurately called myxedema crisis, happens when severe, long-term hypothyroidism reaches a breaking point. Your thyroid isn’t just underperforming-it’s nearly shut down. Without enough thyroid hormone (T3 and T4), your metabolism grinds to a halt. Your heart slows, your lungs barely move, your body temperature drops, and your brain fogs over until you can’t wake up.It’s not a sudden event. Most patients have had undiagnosed or poorly managed hypothyroidism for years. Maybe they were told their fatigue was stress. Maybe their weight gain was blamed on aging. Maybe their cold intolerance was dismissed as being "sensitive." Then something pushes them over the edge-an infection, a missed dose of medication, or a cold snap-and their body can’t compensate anymore.
It’s not just about being tired. It’s about your body literally shutting down. And the scary part? You don’t need to be unconscious to be in crisis. Many patients are just profoundly lethargic, barely responsive, or confused. That’s enough to trigger the emergency protocol.
The Classic Signs You Can’t Afford to Miss
There’s a diagnostic triad that doctors look for: altered mental status, hypothermia, and a triggering event. But in real life, it’s messier.- Altered mental status: This ranges from mild confusion to full coma. Elderly patients often show up as "just not themselves"-slower to respond, withdrawn, or uncooperative. Up to 30% of older adults with myxedema crisis don’t show the classic signs of hypothyroidism. They don’t look like textbook cases.
- Hypothermia: Core body temperature below 35°C (95°F). Not just feeling cold-your body can’t generate heat anymore. This isn’t from being outside in winter. It’s internal failure.
- Bradycardia: Heart rate under 60 bpm, sometimes as low as 30-40. Blood pressure drops. You might have shock without infection.
- Hypoventilation: Breathing rate under 12 breaths per minute. Carbon dioxide builds up. Oxygen levels fall. You can’t breathe well enough to stay alive.
- Non-pitting edema: Swelling in the face, eyelids, lips, and legs. Press on it, and it doesn’t leave a dent. This is the "myxedema" part-the thickening of skin and tissues from mucopolysaccharide buildup.
- GI issues: Ileus (no bowel movement for days), constipation, even megacolon. Digestion stops.
- Hyponatremia: Sodium levels below 135 mmol/L. This isn’t just low salt-it’s a sign your kidneys are failing to regulate fluids properly.
These signs don’t always show up together. That’s why it’s so easy to miss. A 72-year-old woman comes in with pneumonia, low sodium, and a slow heart rate. She’s lethargic. The doctor thinks sepsis. She gets antibiotics. But if you don’t check her thyroid levels, you’re missing the root cause-and the real emergency.
Why Time Is the Enemy
Mortality rates for myxedema coma range from 25% to 60%. That’s higher than diabetic ketoacidosis and close to adrenal crisis. But here’s the key: delayed treatment is the biggest killer.Studies show that for every hour treatment is delayed, the risk of death increases by 10%. Why? Because the body is in multi-organ failure. Your heart can’t pump. Your lungs can’t oxygenate. Your brain is drowning in CO2. Giving thyroid hormone too late means your organs are already too damaged to recover.
Doctors are taught to wait for lab results. That’s the mistake. The American Thyroid Association and Endocrine Society both say: start treatment before the labs come back. If you suspect myxedema coma, give the first dose of thyroid hormone within 30 minutes of suspicion. Don’t wait for TSH or free T4 levels. You won’t have time.
One case from a New Zealand hospital in 2023 involved a woman who missed her levothyroxine for three days after a flu. She was found unresponsive at home. Her temperature was 32.1°C. Her sodium was 128. Her heart rate was 38. She was intubated within 20 minutes of arrival. The first IV levothyroxine dose was given 17 minutes after triage. She woke up 36 hours later. She survived because they didn’t wait.

Emergency Protocol: What to Do Step by Step
There’s a clear, evidence-based sequence. Follow it exactly.- Secure the airway: About 50-70% of patients need intubation. Respiratory failure is common. Don’t wait for apnea. If they’re breathing shallowly, intubate early.
- Give IV thyroid hormone immediately: Start with 300-500 mcg of levothyroxine (T4) intravenously. For severe cases with heart problems, add 10-20 mcg of liothyronine (T3) every 8 hours. The 2022 Endocrine Society update now recommends T3 as first-line in cardiac compromise-it works faster and reduces 30-day mortality by 15%.
- Passive rewarming only: No heating blankets, no warm IV fluids. Active rewarming can cause sudden vasodilation and cardiac arrest. Cover them with blankets. Let their body warm up slowly as hormone levels rise.
- Treat the trigger: Infection is the cause in 30-50% of cases. Start broad-spectrum antibiotics right away-even if you’re not sure. Pneumonia and UTIs are the most common. Don’t wait for cultures.
- Correct electrolytes slowly: If sodium is low, correct it by no more than 4-6 mmol/L in the first 24 hours. Too fast can cause brain damage from osmotic demyelination.
- Monitor continuously: Core temperature every 30 minutes. Blood gases every 2-4 hours. Cardiac rhythm. Urine output. These patients are unstable. They need ICU-level care.
Use the DIMES mnemonic to find triggers: Drugs (medication non-adherence, sedatives), Infection, Myocardial infarction or stroke, Exposure to cold, Stroke. If one of these is present, it’s likely the spark.
What Not to Do
There are dangerous myths in emergency medicine.- Don’t give corticosteroids without checking adrenal function. Hypothyroidism can mask adrenal insufficiency. Giving steroids without knowing cortisol levels can cause sudden collapse. Test cortisol before giving hydrocortisone.
- Don’t use active warming. As mentioned, it can trigger fatal arrhythmias.
- Don’t wait for TSH to be "high enough". TSH can be over 100 mIU/L-but even a TSH of 20 with low T4 and clinical signs is enough to treat.
- Don’t assume it’s just depression. Especially in older women. "Apathetic hypothyroidism" is real. No tremors, no weight gain, no dry skin-just confusion and lethargy.
Who’s at Risk?
Myxedema coma is rare-only 0.2 to 0.6 cases per million people each year. But it’s not random.- Women over 60: 3 times more likely than men.
- People with Hashimoto’s thyroiditis: The most common cause of hypothyroidism.
- Those who miss doses: Especially during hospital stays or illness. One patient in a 2022 survey stopped thyroid meds after a hospital admission for pneumonia-and ended up in ICU for 11 days.
- People in cold climates: Scandinavian countries report 50% higher rates than Mediterranean regions.
- Uninsured or underinsured patients: They wait longer to seek care. Time-to-treatment is 35% longer. Mortality is 22% higher.
Men are less likely to get it-but when they do, they’re more likely to be misdiagnosed. One study found men account for 25% of cases but 40% of diagnostic delays. Symptoms get written off as "just getting older."
What’s New in Treatment?
The field has evolved. In 2023, the FDA approved a new IV thyroid hormone formulation called Thyrogen®, which absorbs faster than older versions. That’s important when you’re racing against time.Research is also moving toward early detection. A 2023 Lancet study found that elevated thyrotropin receptor antibodies can predict decompensation before coma sets in-with 85% sensitivity. That’s huge. Imagine a blood test that tells you someone is about to crash, weeks before it happens.
Point-of-care thyroid tests are in phase 3 trials. These devices can give you TSH and free T4 results in 15 minutes at the bedside. In the future, ER doctors won’t wait hours for labs. They’ll know within minutes.
Why This Matters Beyond the ICU
Myxedema coma is the tip of the iceberg. Behind every case is a person who went undiagnosed or undertreated for years. It’s a failure of primary care, of patient education, of awareness.Patients on thyroid medication need to know: if you get sick, don’t stop your pills. If you’re hospitalized, remind the staff you’re on thyroid hormone. If you’re cold, tired, and confused-don’t accept "it’s just aging."
Doctors need to know: if an elderly patient has unexplained low sodium, slow heart rate, or mental changes-check the thyroid. It takes 30 seconds. It could save a life.
The aging population means this condition will get more common. The Global Burden of Disease Study predicts a 20% rise in cases by 2030. We need better screening, better education, and faster protocols. Not just in big hospitals-but in clinics, nursing homes, and emergency rooms everywhere.
Can myxedema coma happen to someone who’s been on thyroid medication?
Yes. In fact, many cases occur in people already on levothyroxine. Missing doses-even for a few days-can trigger decompensation, especially during illness, surgery, or cold exposure. Hospitalizations are a major risk. Always inform medical staff you’re on thyroid medication, and never stop it without direction.
Is myxedema coma the same as thyroid storm?
No. They’re opposites. Thyroid storm is caused by too much thyroid hormone-leading to high fever, rapid heartbeat, and agitation. Myxedema coma is caused by too little-leading to low temperature, slow heart rate, and lethargy. Treatment is completely different. Thyroid storm uses antithyroid drugs; myxedema coma needs thyroid hormone replacement.
How long does it take to recover from myxedema coma?
Recovery varies. Mental status often improves within 24-48 hours after starting hormone therapy. Body temperature and heart rate normalize over several days. Full recovery can take weeks, especially if there was organ damage. But patients who get treatment early often return to their baseline function.
Can you prevent myxedema coma?
Yes. Regular thyroid function tests, consistent medication use, and prompt treatment of infections are key. Patients should have a plan for illness-like increasing their dose temporarily during infection, under doctor supervision. Educating patients about warning signs-like extreme fatigue, confusion, or unexplained cold sensitivity-can prevent crisis.
Why is hyponatremia common in myxedema coma?
Low thyroid hormone reduces the kidney’s ability to excrete free water. This leads to water retention and diluted sodium levels. It’s not caused by dehydration or salt loss-it’s a hormonal imbalance. Correcting it too quickly can damage the brain, so it must be done slowly.
Is myxedema coma more common in winter?
Yes. Cold exposure worsens hypothyroidism by increasing the body’s demand for heat production-which the thyroid can’t meet. Studies show higher incidence in colder regions and during winter months. Patients with hypothyroidism should be warned to avoid prolonged cold exposure and to keep their homes warm.

Prem Hungry
bro this is wild i had my grandma in ICU last year with this and no one checked her TSH till day 3... she was just "being old" until her lips turned blue. now she’s back home eating roti and yelling at the TV. check thyroids people. it’s free.
Leslie Douglas-Churchwell
Let’s be real - this isn’t medicine. It’s corporate endocrinology propaganda. The FDA approved Thyrogen®? That’s a patent extension disguised as innovation. The real crisis is Big Pharma’s monopoly on T3/T4 formulations. Meanwhile, patients in rural India are crushing desiccated thyroid pills from black-market pharmacies and thriving. Wake up. The system is rigged. 🤫💊
shubham seth
Myxedema coma is basically the thyroid’s middle finger to your body’s entire operating system. You think you’re just tired? Nah. You’re one missed pill away from becoming a human Popsicle with a heartbeat that sounds like a dying dial-up modem. And don’t get me started on how docs treat elderly women like walking ghosts. ‘Oh honey, you’re just depressed.’ Nah. You’re a walking lab report waiting to explode.
Kathryn Ware
This is such an important post - thank you for laying it out so clearly. I’m a nurse in a rural ER and we see this way more than people think. Last month, a 74-year-old woman came in with ‘just a cold’ and a heart rate of 39. We didn’t wait for labs - gave her 500 mcg IV T4 on sight, started antibiotics, and she was coherent by morning. The key is trusting clinical signs over waiting for numbers. Also - passive rewarming is non-negotiable. I’ve seen people die from heating blankets. Please, everyone, share this. It’s literally life-saving knowledge. ❤️🫂
kora ortiz
STOP WAITING. CHECK THE THYROID. IF THEY’RE SLOW, COLD, CONFUSED - GIVE THE HORMONE. NO EXCUSES. NO LABS. NO ‘LET’S OBSERVE.’ THIS ISN’T A DEBATE. IT’S A CODE BLUE WITH A DIFFERENT NAME. YOU HAVE 30 MINUTES. ACT. NOW. 🚨
Jeremy Hernandez
Y’all are acting like this is new info. It’s been in textbooks since the 90s. The real problem? Lazy docs. I’ve seen people die because the ER doc was too busy scrolling TikTok to check TSH. Also - ‘Thyrogen®’? That’s just a rebranded T4 with a fancy label. Same damn drug. Stop falling for pharma marketing. And no, cold weather doesn’t cause it - poor healthcare access does.
Tarryne Rolle
Is this not just another example of how medicine pathologizes the natural decline of the human body? We’ve turned aging into a disease to be fixed with hormones. What if the body is simply… slowing down? What if the silence, the cold, the stillness - is not failure, but surrender? We rush to revive what nature intended to fade. Isn’t that arrogance dressed in white coats?
Kyle Swatt
I’ve sat with people in the ICU during these crises. You see the family staring at the monitor like it’s a fortune teller. The silence is heavier than the machines. This isn’t just physiology - it’s a story of neglect. Missed appointments. Unaffordable meds. Elders told to ‘tough it out.’ We treat the hormone but ignore the human. The real crisis isn’t the coma - it’s the years of silence before it.
Deb McLachlin
Thank you for the comprehensive overview. I am particularly interested in the 2023 Lancet study regarding thyrotropin receptor antibodies as predictive markers. Could you provide a link to the publication or the DOI? Additionally, are there any ongoing trials in Canada for point-of-care thyroid testing that are publicly documented? This has significant implications for primary care screening protocols in aging populations.
saurabh lamba
why do we even need all this? just give people thyroid pills and stop acting like its rocket science. my cousin took his meds and lived. others didn't. simple. now go drink your tea.
Elia DOnald Maluleke
Let me tell you about the man in Durban who survived myxedema coma after drinking ginger tea and chanting mantras for three days. The hospital gave him T4 - but he credits his grandmother’s herbal poultice. Science may measure hormones, but the soul measures survival. We forget: healing is not always in the vial. Sometimes, it’s in the hands that held you when you couldn’t speak.
satya pradeep
bro i work in a clinic in hyderabad and we’ve started giving TSH strips to patients over 60 during flu season - just 2 bucks. if it’s above 20? send ‘em to hospital. saved 3 lives this year. also - if your grandma stops her pills when she’s sick? she’s gonna die. tell her. tell everyone. this ain’t drama. it’s math. no T4 = no life. simple.
Kiran Mandavkar
What’s next? Will we start labeling depression as ‘apathetic hypothyroidism’ and prescribing T4 to people who just hate their jobs? This is medical imperialism disguised as compassion. You’re reducing existential fatigue to a hormone imbalance. What about the people who are tired because the world is burning? Fix the system, not the thyroid.