Many people take quercetin supplements hoping to reduce inflammation, fight allergies, or boost immunity. But what they don’t realize is that this popular flavonoid can quietly change how their medications work - sometimes dangerously. If you’re on blood thinners, heart drugs, antidepressants, or cancer treatments, taking quercetin could raise your drug levels by 30% to over 300%. That’s not a small risk. It’s the difference between a safe dose and a toxic one.
What Quercetin Does to Your Liver’s Drug-Metabolizing System
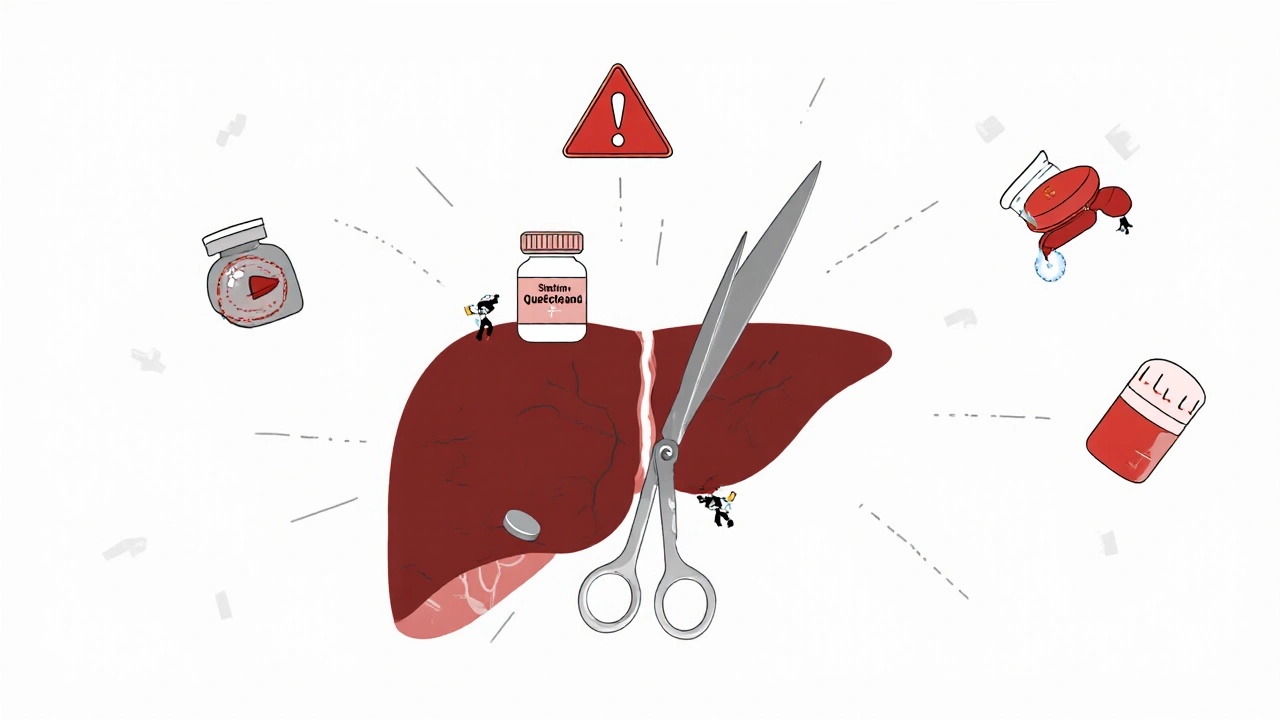
Your liver uses enzymes called cytochrome P450 (CYP) to break down most medications. Think of them as tiny scissors that chop drugs into pieces so your body can flush them out. Quercetin doesn’t just sit there - it jams those scissors. Research shows it strongly blocks CYP2D6 and CYP2C19, and moderately blocks CYP3A4. These three enzymes handle more than 70% of all prescription drugs.
At just 10 micromolar concentration - the kind you get from a 500 mg supplement - quercetin cuts CYP2D6 activity by 70-85%. That’s nearly as strong as the drug quinidine, which is used specifically to inhibit this enzyme. For CYP3A4, it cuts metabolism by 40-60%. That’s enough to make drugs like statins, blood pressure pills, or immunosuppressants build up in your blood.
And it’s not just enzymes. Quercetin also blocks transporters like OATP1B1 and BCRP, which control how drugs enter and leave your liver and intestines. This means even if your liver could break down the drug, quercetin might stop it from getting there in the first place - or trap it in your system longer than it should stay.
Which Medications Are Most at Risk?
Not all drugs are affected the same. Some are extremely sensitive to even small changes in metabolism. Here are the ones you need to watch out for:
- Warfarin: Quercetin can raise INR levels by 0.8 to 1.5 points - enough to cause internal bleeding. There are documented cases of patients on warfarin needing emergency treatment after starting quercetin.
- Cyclosporine and tacrolimus: These transplant drugs have a razor-thin safety window. Quercetin can raise their levels by 30-50%, leading to kidney damage or nerve toxicity.
- Abemaciclib, abrocitinib: Cancer and eczema drugs metabolized by CYP3A4. Quercetin increases their blood levels by 25-50%, raising the risk of severe low blood counts or infections.
- Acenocoumarol: Another blood thinner. Studies show 30-45% higher levels when taken with quercetin.
- Apixaban and rivaroxaban: Newer blood thinners (DOACs). Quercetin’s effect on transporters increases their exposure by 20-35%, and the American Society of Health-System Pharmacists says to avoid quercetin entirely with these.
- Antidepressants like sertraline or fluoxetine: Metabolized by CYP2D6. Quercetin can cause dizziness, nausea, or even serotonin syndrome.
- Acetaminophen: Even common painkillers can become riskier. Quercetin increases their levels by 20-30%, which may raise liver stress in people who already take high doses.
Supplements vs. Food: Why It Matters
Don’t panic if you eat apples, onions, or capers. The quercetin in food is bound to sugar molecules (glycosides like rutin), and your body absorbs it slowly and poorly. Less than 5% of dietary quercetin even enters your bloodstream.
But supplements? They’re different. Most use the pure aglycone form - the kind your body absorbs quickly and in high amounts. A 500 mg supplement delivers 100 times more active quercetin than a cup of onions. And many people take 1,000 mg or more daily, believing more is better.
According to the 2021 National Health Interview Survey, 42% of Americans taking quercetin supplements use over 500 mg per day. 23% take more than 1,000 mg. That’s not a health boost - it’s a pharmacological intervention. And it’s happening without any medical oversight.

Who’s Most at Risk?
It’s not just about how much you take. Your body matters too.
- People over 65: They clear quercetin 25-40% slower than younger adults. That means the compound builds up faster and stays longer.
- People on multiple medications: If you’re taking five or more drugs, the chance of one being affected by quercetin jumps dramatically. Polypharmacy turns a small interaction into a medical emergency.
- People with liver or kidney disease: If your organs are already struggling to process drugs, quercetin pushes them over the edge.
- Patients with cancer or autoimmune conditions: Many of these drugs have narrow therapeutic windows. Even a 20% rise in concentration can trigger serious side effects.
One study in rats showed midazolam (a sedative) levels jumped 2.3 times when given with quercetin. That’s not theoretical. It’s what happens in real human bodies - especially when taken on an empty stomach or with high doses.
What Experts Are Saying
The European Food Safety Authority (EFSA) warned in 2018 that quercetin supplements above 1,000 mg/day pose “potential concerns” for drug interactions. The FDA listed quercetin as a “dietary supplement of concern” in its 2020 draft guidance, specifically calling out CYP3A4, CYP2D6, and CYP2C19.
Dr. Basheer Kerem, a pharmacologist at Hebrew University, says intestinal CYP3A4 inhibition may be even more dangerous than liver effects - because that’s where drugs are first absorbed. If quercetin blocks the enzyme right in the gut, you get a massive spike in drug levels before it even reaches your bloodstream.
And here’s the kicker: the FDA has logged 147 suspected quercetin-drug interaction cases since 2015. But they estimate 90-95% go unreported. That means thousands of people could be experiencing side effects without knowing why.

What Should You Do?
If you’re taking any prescription medication, here’s what to do:
- Stop taking quercetin supplements if you’re on blood thinners, transplant drugs, cancer meds, or antidepressants.
- Talk to your pharmacist. They have access to drug interaction databases and can check your specific meds. Don’t rely on your doctor alone - pharmacists specialize in this.
- If you must take it, keep the dose under 250 mg/day and take it at least 6 hours apart from your medication. Studies show this cuts interaction risk by 30-50%.
- Never start or stop quercetin without telling your healthcare provider. Even if you think it’s “just a supplement.”
- Watch for signs of toxicity: Unusual bruising, dizziness, extreme fatigue, confusion, nausea, or irregular heartbeat. These could be early signs your drug levels are too high.
The bottom line: Quercetin isn’t harmless. It’s a potent biochemical agent. And when you combine it with medication, you’re playing with fire - even if you think you’re just being “natural.”
What’s Changing in the Future?
The FDA is working on a 2024 rule that would require supplement labels to warn about drug interactions - especially for high-risk ingredients like quercetin. Clinical trials (NCT04873325, NCT04659262) are now underway to pin down exact safe dosing levels.
Until then, assume the worst. If you’re on medication, don’t take quercetin supplements unless your doctor or pharmacist has approved it - and even then, monitor closely.
Your health isn’t a gamble. Don’t risk it for a supplement that’s not worth the danger.
Can I take quercetin if I’m on blood thinners?
No. Quercetin increases the levels of warfarin, acenocoumarol, apixaban, and rivaroxaban by 20-50%, which raises your risk of serious bleeding. The American Society of Health-System Pharmacists recommends avoiding quercetin entirely if you’re on any blood thinner. Even small doses can be dangerous.
Is quercetin from food safe?
Yes. The quercetin in apples, onions, capers, and berries is bound to sugar molecules and poorly absorbed. You’d need to eat over 10 cups of onions daily to reach the same blood levels as a 500 mg supplement. Dietary intake does not pose a meaningful interaction risk.
How much quercetin is too much?
For people on medications, any dose over 250 mg per day is risky. The European Food Safety Authority flags doses above 1,000 mg/day as having “potential concerns.” Most supplement users take 500-1,000 mg, which is enough to interfere with drug metabolism. If you’re on any prescription drug, stay under 250 mg - or avoid it entirely.
Can I take quercetin at a different time than my meds?
Spacing quercetin and your medication by 4-6 hours can reduce interaction risk by 30-50%, according to clinical pharmacology studies. But this doesn’t eliminate the risk - especially for drugs with narrow therapeutic windows. It’s safer to avoid quercetin entirely if you’re on critical medications.
Are all quercetin supplements the same?
No. Most supplements use pure quercetin aglycone, which is highly bioavailable and potent. Some use rutin (quercetin glycoside), which is weaker and safer - but many labels don’t specify. Check the ingredient list: if it says “quercetin,” assume it’s the strong form. If it says “rutin,” it’s safer - but still not risk-free with sensitive drugs.
Why don’t doctors warn patients about this?
Many doctors aren’t trained in supplement interactions. Supplements aren’t regulated like drugs, so they’re often overlooked. But pharmacists and clinical toxicologists are aware. If you’re on multiple medications, ask your pharmacist to review everything you’re taking - including vitamins and herbs.
Is quercetin safe for healthy people not on meds?
For healthy adults not taking any medications, short-term use of up to 500 mg/day appears safe based on current data. But long-term safety data is limited. There’s no proven benefit for healthy people that outweighs the potential risks - especially since you can get all the quercetin you need from food.
Jennifer Walton
Quercetin isn’t magic. It’s just another molecule with unintended consequences. We treat supplements like tea, but they’re pharmacologically active. That’s the problem.
Kihya Beitz
Oh great. Another ‘natural’ thing that’s actually a stealth drug. Next they’ll tell us broccoli causes liver failure. 😒
Edward Ward
This is exactly why we need better public education on pharmacokinetics - not just fear-mongering. The science here is solid: CYP enzyme inhibition is well-documented, and the dose-response curve for quercetin is terrifyingly steep. But here’s the nuance: not everyone metabolizes drugs the same way. Genetic polymorphisms in CYP2D6 alone mean some people are ultra-rapid metabolizers, others are poor - so the risk isn’t uniform. And while supplements are unregulated, the fact that 42% of users take over 500mg daily? That’s not ‘natural wellness,’ that’s self-prescribed pharmacology. We need labeling standards, not just warnings. And pharmacists? They’re the unsung heroes here. If you’re on more than three meds, you owe it to yourself to sit down with one. Not your doctor - your pharmacist. They see these interactions every day.
Andrew Eppich
People take supplements like they’re candy. No prescription. No oversight. No consequences. And then they wonder why they end up in the ER. This isn’t ‘alternative medicine.’ It’s reckless. If you can’t trust your body to handle food, why would you trust a pill from a company that doesn’t even have to prove safety? Common sense is dying.
Jessica Chambers
My aunt took quercetin with her blood thinner... and ended up in the hospital. 🙃 I told her it was ‘just a supplement.’ Turns out, it’s not.
Shyamal Spadoni
Big Pharma doesn't want you to know this because they profit off the drugs that quercetin interferes with! They’ve been suppressing studies since the 90s! The FDA is a puppet of the pharmaceutical lobby - they only ‘warn’ now because they’re forced to. Quercetin is nature’s way of balancing the system - they just don’t want you to have free medicine. And don’t get me started on how they chemically alter the food supply to make you dependent on pills - onions are now ‘toxic’ because they’re too natural. Wake up!
Ogonna Igbo
Why are Americans so scared of natural things? In Nigeria, we use herbs for everything - and we don’t end up in hospitals. You people take a pill for a sneeze. Now you’re scared of a plant compound? This is why your healthcare costs are insane. Quercetin is from onions. Onions. You eat them. You don’t panic. Why are you so weak? You need to stop treating your body like a broken machine.
BABA SABKA
Let’s be real - the real issue isn’t quercetin. It’s polypharmacy. If you’re on five meds, you’re already playing Russian roulette. Quercetin just exposes the mess. And the fact that doctors don’t ask about supplements? That’s the real failure. I’ve seen patients on 12 pills, no one checks for herbals. The system is broken. Quercetin is just the symptom. Fix the damn system before you blame the supplement.
Chris Bryan
They’re coming for all supplements next. First quercetin, then vitamin D, then magnesium. This is how they control us. You think they care about your liver? No. They care about your wallet. Every time you use a natural remedy, you’re stealing their profit. So they scare you with ‘interactions’ - because they can’t compete with something that costs $10 and comes from a tree.
Jonathan Dobey
Quercetin is the phoenix of flavonoids - ancient, potent, and misunderstood. It doesn’t ‘interfere’ with drugs - it *rebalances* the system. The liver isn’t a factory, it’s a symphony. And CYP enzymes? They’re just the violins. Quercetin isn’t jamming the scissors - it’s turning down the volume so the body can hear its own rhythm. But modern medicine? It only understands brute force. Pills to kill, pills to replace, pills to mask. They don’t understand harmony. And now they’re criminalizing the quiet healer because it doesn’t come in a patentable capsule. The real danger isn’t quercetin - it’s the arrogance of a system that thinks it owns biology.
ASHISH TURAN
My dad takes warfarin and started quercetin after reading a blog. INR went from 2.1 to 4.8 in two weeks. No symptoms until he bruised his thigh for no reason. Got admitted. Now he’s off it. Don’t assume it’s safe just because it’s ‘natural.’ Always check with your pharmacist. Simple.
Ryan Airey
Anyone who takes over 500mg of quercetin daily without medical supervision is either dangerously naive or actively trying to harm themselves. This isn’t ‘biohacking.’ It’s self-sabotage. And the fact that supplement companies don’t list drug interaction warnings? That’s criminal negligence. If you’re not a pharmacologist, don’t play chemist.
Hollis Hollywood
I’ve been reading this whole thing and I just feel so sad. People are scared to take anything - even things that might help - because the system is so broken. We’ve turned health into a minefield of warnings, but no one gives you the tools to navigate it. I get the science. I really do. But what’s the alternative? Do we just say ‘don’t take anything’? What about the person who’s been taking quercetin for years with no issues? What about the one who’s allergic to everything else? We need more than fear. We need guidance. We need access to pharmacists who can sit with you and say, ‘Here’s your risk profile.’ Not a blog post. Not a label. A conversation. That’s what’s missing.