Every year, millions of people take over-the-counter (OTC) medicines without thinking twice. A headache? Grab some ibuprofen. Trouble sleeping? A diphenhydramine pill does the trick. But what if you’re already on a prescription drug for high blood pressure, depression, or heart disease? That’s when things get dangerous - and most people don’t realize it until it’s too late.
Why OTC Medications Are Riskier Than You Think
You don’t need a prescription to buy them, but that doesn’t mean they’re harmless. OTC meds like painkillers, sleep aids, antacids, and cold remedies can change how your prescription drugs work - sometimes in life-threatening ways. The biggest problem? Most people never tell their doctor or pharmacist what they’re taking. A WebMD survey found that 67% of patients don’t mention their OTC use. That means your doctor might think you’re on just one blood thinner, when you’re also taking daily ibuprofen for back pain. The result? A 2- to 4-times higher risk of internal bleeding. Even common OTC products like acetaminophen (Tylenol) can cause liver failure if you accidentally double up. Many cold medicines, flu remedies, and sleep aids contain acetaminophen. If you take one for your cough and another for your headache, you could easily hit 7,000 mg in a day - almost double the safe limit of 4,000 mg.Top 5 Dangerous Combinations You Need to Avoid
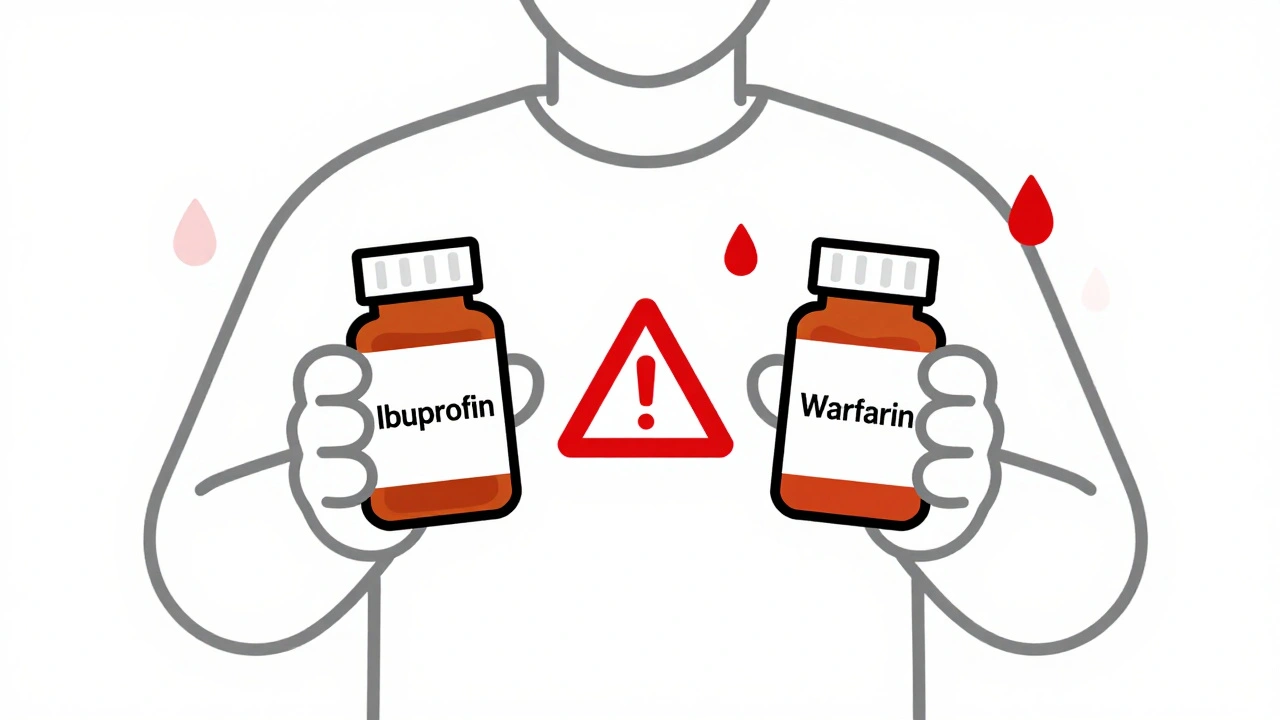
Not all OTC meds are equally risky. Some combinations are known to cause serious harm. Here are the five most dangerous ones you need to watch out for:- NSAIDs (ibuprofen, naproxen) + blood thinners (warfarin, apixaban): These can cause severe internal bleeding. NSAIDs thin the blood on their own. Add them to a prescription anticoagulant, and your risk of bleeding skyrockets.
- NSAIDs + blood pressure meds (lisinopril, losartan): NSAIDs can make these drugs less effective. Your blood pressure might spike by 5-15 mmHg - enough to trigger a stroke or heart attack in someone already at risk.
- SSRIs (sertraline, fluoxetine) + dextromethorphan (cough syrup): Both affect serotonin. Together, they can cause serotonin syndrome - a rare but deadly condition with symptoms like confusion, rapid heartbeat, high fever, and seizures.
- Antacids (Tums, Maalox) + levothyroxine (thyroid med): Aluminum and magnesium in antacids bind to thyroid medication, cutting its absorption by up to 25%. That means your thyroid levels stay low, even if you’re taking your pill every morning.
- Acetaminophen + alcohol or liver disease: Even moderate alcohol use with acetaminophen can damage your liver. If you have fatty liver disease or drink regularly, your liver can’t process the drug safely. One extra pill a day for a week might be all it takes.
What About Supplements and Herbal Remedies?
You might think “natural” means safe. It doesn’t. Garlic, ginkgo, and ginseng can all interfere with blood thinners. St. John’s Wort - often taken for mild depression - can make birth control pills, antidepressants, and even heart meds stop working. Multivitamins aren’t harmless either. Iron, calcium, and magnesium in supplements can block absorption of antibiotics like tetracycline or osteoporosis drugs like alendronate. Take them at the same time? You’re wasting your prescription.Who’s at Highest Risk?
Some people are far more likely to have dangerous interactions:- Elderly patients: The average person over 65 takes 5 or more medications daily. OTC meds get added on top - often without review.
- People with kidney or liver disease: These organs clear drugs from your body. If they’re not working well, even normal doses can build up to toxic levels.
- Those on multiple prescriptions: If you’re taking three or more drugs, your risk of interaction jumps dramatically.
- People with chronic conditions: High blood pressure, diabetes, heart disease, and depression all come with meds that react badly to common OTCs.
How to Protect Yourself - A Simple Checklist
You don’t need to be a doctor to avoid these risks. Just follow these steps before you take any OTC medicine:- Read every label. Look for active ingredients - not just brand names. If two products say “acetaminophen” or “ibuprofen,” don’t take both.
- Keep a written list. Write down every pill, capsule, or syrup you take - including vitamins, herbs, and supplements. Include the reason you take it and the dose.
- Ask your pharmacist. Pharmacists are trained to spot interactions. Bring your list every time you pick up a new prescription. They’ll tell you if something’s risky.
- Check before you buy. Use free tools like WebMD’s Drug Interaction Checker. Type in your prescription and the OTC drug you’re thinking of taking. It’ll flag dangers instantly.
- Never assume “it’s just a cold pill”. Even a single dose of an OTC decongestant can raise your blood pressure if you’re on a beta-blocker.

What to Do If You’ve Already Mixed Them
If you’ve taken an OTC med with your prescription and feel off - dizzy, nauseous, confused, or if you notice unusual bruising, dark stools, or rapid heartbeat - don’t wait. Call your doctor or go to urgent care. Don’t wait until tomorrow. If you’re unsure whether you’ve taken too much acetaminophen, get checked. Liver damage can happen without symptoms at first. A simple blood test can catch it early.Why This Keeps Happening - And What’s Changing
The problem isn’t just ignorance. OTC labels are confusing. Small print, vague warnings, and inconsistent formatting make it hard to spot risks. In 2022, the FDA started pushing for clearer labeling on high-risk OTC products - especially those linked to liver damage or bleeding. Hospitals are also starting to ask patients about OTC use during intake. But until patients start speaking up, the system won’t fix itself. The good news? More pharmacies now offer free medication reviews. You don’t need an appointment. Just walk in with your list. They’ll check for interactions, suggest safer alternatives, and even help you organize your pills.Final Thought: Your Health Isn’t a Guessing Game
OTC meds are convenient. But convenience shouldn’t come at the cost of your safety. The same care you take with your prescription drugs should apply to everything you swallow - even if it’s on a shelf next to gum and cough drops. If you’re unsure, pause. Ask. Check. It’s not overcautious - it’s smart.Can I take ibuprofen with my blood pressure medicine?
It depends. Ibuprofen and other NSAIDs can reduce the effectiveness of blood pressure medications like lisinopril or losartan. They may also raise your blood pressure by 5-15 mmHg. If you have heart disease or kidney issues, this can be dangerous. Talk to your pharmacist before taking ibuprofen. Acetaminophen is often a safer pain relief option for people on blood pressure meds.
Is it safe to take Tylenol with antidepressants?
Acetaminophen (Tylenol) generally has fewer interactions than NSAIDs, and it’s usually safe with most antidepressants. But if you’re taking an SSRI like sertraline or fluoxetine and also using other serotonin-affecting drugs (like dextromethorphan in cough syrup), you could risk serotonin syndrome. Always check the full list of ingredients in any OTC product you take with antidepressants.
Why do antacids interfere with thyroid medication?
Antacids containing aluminum or magnesium bind to levothyroxine in your gut, preventing your body from absorbing it. This can make your thyroid medication ineffective - even if you’re taking it exactly as prescribed. To avoid this, take your thyroid pill on an empty stomach, at least 4 hours before or after any antacid, calcium supplement, or multivitamin.
Can I take melatonin with my sleep prescription?
Melatonin is often considered safe, but combining it with prescription sleep aids like zolpidem or benzodiazepines can increase drowsiness, dizziness, and the risk of falls - especially in older adults. It can also affect your body’s natural sleep cycle. Always check with your doctor before mixing melatonin with any sleep medication.
How do I know if I’ve taken too much acetaminophen?
Early signs of acetaminophen overdose are mild - nausea, vomiting, loss of appetite, and tiredness. But liver damage can be silent for days. If you’ve taken more than 4,000 mg in 24 hours - especially if you’ve been drinking alcohol or have liver disease - get a blood test. Don’t wait for symptoms. The sooner you’re treated, the better your chances of recovery.
Should I stop taking OTC meds before my doctor’s appointment?
No. Bring them with you. Your doctor needs to know exactly what you’re taking - even if you only use it once a month. Stopping suddenly could hide a real interaction. Instead, write down everything: brand names, doses, how often you take it, and why. That’s the best way to keep yourself safe.
Ben Greening
It’s staggering how many people treat OTC meds like candy. I’ve seen patients take ibuprofen daily for years without realizing it’s undermining their lisinopril. The real issue isn’t the drugs-it’s the cultural assumption that ‘if it’s on a shelf, it’s harmless.’
Pharmacists are the unsung heroes here. They see the full picture. If you walk in with a list, they’ll catch what your doctor might miss.
Clear labeling is long overdue. The FDA’s recent push is a start, but it needs teeth. Retailers should be required to highlight high-risk combinations in bold at point-of-sale.
Nikki Smellie
Have you ever wondered why Big Pharma doesn’t want you to know this? 🤔
They profit from dependency. OTC meds are the gateway drug to lifelong prescriptions. That’s why they bury the warnings in 6-point font and call it ‘consumer freedom.’
They don’t want you asking questions. They want you swallowing pills without thinking. The FDA? Controlled by lobbyists. Your pharmacist? Paid to upsell. Your doctor? Overworked and out of the loop.
Only YOU can protect yourself. Keep a binder. Photograph every bottle. Track every interaction. And never trust a label again. 🚨💊
David Palmer
Man, I just took a Tylenol for my headache and I’m on blood pressure meds. Should I be freakin’ out? 😅
Also, why do they put acetaminophen in everything? Cold medicine? Sleep aid? Painkiller? It’s like they’re trying to kill us slowly.
My grandma takes Tums with her thyroid pill and swears she’s fine. Maybe she’s just lucky?
Doris Lee
This is such an important topic-thank you for sharing it so clearly.
I used to think OTC meant ‘no big deal,’ but after my dad had a bleed from mixing ibuprofen and warfarin, I learned the hard way.
Now I keep a little card in my wallet with all my meds and supplements. I show it to every pharmacist. It’s a tiny habit, but it saves lives.
You don’t have to be a doctor to be safe. Just be curious. And speak up.
And if you’re unsure? Pause. Ask. Check. It’s not overcautious-it’s love for yourself.
Michaux Hyatt
Great breakdown. I work in community health, and this is the #1 thing we educate patients on.
One trick: if you’re on more than three meds, schedule a free med review at your pharmacy every six months. No appointment needed.
Also-people forget that supplements count. St. John’s Wort isn’t ‘natural’-it’s a potent enzyme inducer. It can tank your birth control, antidepressants, even statins.
Don’t assume ‘herbal’ = ‘safe.’ It just means it’s unregulated.
And yes, melatonin with zolpidem? Big no. Drowsiness isn’t the only risk-it’s impaired coordination. Falls in seniors are deadly.
Jack Appleby
Let’s be precise: the real problem isn’t ignorance-it’s the pathological commodification of pharmacology.
OTC medications are engineered for impulse consumption, their labeling deliberately obfuscated to maximize volume and minimize liability. The FDA’s recent labeling initiatives are performative-they lack enforcement mechanisms and fail to address systemic incentives.
Furthermore, the conflation of ‘natural’ with ‘safe’ is a dangerous semantic fallacy rooted in romanticized pseudoscience. Ginkgo biloba is not a ‘herb’-it’s a potent antiplatelet agent. Ginseng modulates CYP3A4. These are not benign botanicals-they are bioactive compounds with pharmacokinetic profiles.
And yes, the 4,000 mg acetaminophen ceiling is a myth-it’s 3,000 mg for chronic users, and 2,000 mg if you consume alcohol. The FDA’s guidelines are outdated. The literature is clear.
Frank Nouwens
Well-structured and thoroughly researched. The inclusion of specific pharmacokinetic interactions-such as aluminum/magnesium binding to levothyroxine-is particularly valuable.
It’s worth noting that the 4-hour separation window between antacids and thyroid medication is not universally accepted; some studies suggest 2 hours may suffice in healthy individuals. However, given the variability in gastric pH and motility, erring on the side of caution is prudent.
I would also recommend that patients use a pill organizer with labeled compartments, especially if they’re managing multiple daily regimens. Visual cues reduce error rates by up to 40% in elderly populations.
Thank you for elevating this critical public health issue.
Queenie Chan
What if the real danger isn’t the drugs-but the way we’ve been taught to think about them?
We’ve turned medicine into a transaction: symptom → pill → relief. But the body isn’t a vending machine. It’s a network. A cascade. A conversation between thousands of molecules.
When you take ibuprofen with warfarin, you’re not just ‘adding a pill.’ You’re altering the balance of clotting factors, endothelial function, platelet aggregation.
And we don’t even know half of what’s happening. Most OTC interactions aren’t studied in real-world polypharmacy populations. We’re flying blind.
Maybe the solution isn’t just more labels-but a cultural shift. From ‘take it if it helps’ to ‘understand why it works.’
Stephanie Maillet
...and yet, we keep doing it...
Because we’re tired. Because we’re in pain. Because we’re scared. Because we don’t know who to trust. Because the system doesn’t make it easy.
It’s not just about reading labels-it’s about being heard. About having someone sit with you, not just scan your list.
My mother took Tums with her thyroid med for years. She didn’t know. No one asked. No one explained.
And now? She’s on a higher dose. And still, she doesn’t feel right.
Maybe the real medicine isn’t in the bottle.
Maybe it’s in the conversation.
...and we’ve forgotten how to have them.
Kaitlynn nail
So… just don’t take anything. Ever. 🤷♀️