Medication Interaction Checker
Check Medication Interactions
Enter your medication name to see if it interacts with acid-reducing drugs like omeprazole, famotidine, or ranitidine.
Many people take acid-reducing medications like omeprazole, esomeprazole, or ranitidine for heartburn or stomach ulcers. But what most don’t realize is that these drugs can quietly sabotage the effectiveness of other medications they’re taking. It’s not a rare side effect-it’s a well-documented, widespread problem that affects thousands of patients every year.
How Acid-Reducing Medications Work
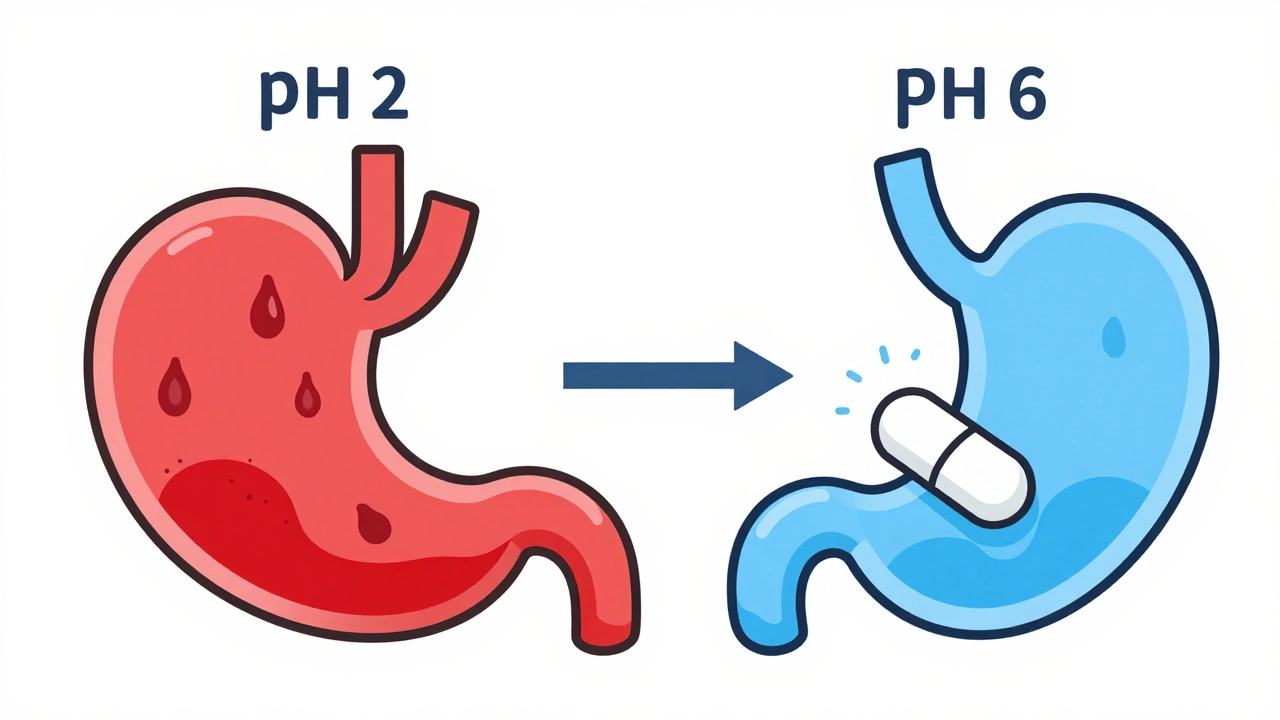
Proton pump inhibitors (PPIs) and H2-receptor antagonists (H2RAs) reduce stomach acid by targeting different parts of the acid-production system. PPIs like omeprazole shut down the final step of acid secretion in stomach cells, keeping gastric pH elevated for 14 to 18 hours a day. H2RAs like famotidine block histamine signals that trigger acid release, raising pH for about 8 to 12 hours. Normal stomach acid ranges from pH 1.0 to 3.5 when fasting. When you take these drugs, that level jumps to 4.0-6.0-sometimes even higher.
This change sounds harmless, but it’s enough to mess with how your body absorbs other pills. Most drugs don’t dissolve well in acid-free environments. That’s especially true for weakly basic drugs-medications that rely on stomach acid to dissolve properly before moving into the small intestine.
The Science Behind the Interference
Drug absorption follows the Henderson-Hasselbalch equation, which predicts how a drug’s ionization changes with pH. Weakly basic drugs (those with a pKa above 7) become less soluble when stomach acid drops. Instead of dissolving and being absorbed, they clump together and pass through the gut unchanged.
Think of it like salt in water. Salt dissolves easily in cold water, but not so well in oil. In the same way, certain drugs need acid to dissolve. When you take a PPI, you’re essentially turning your stomach into an oil bath for those drugs.
Research shows that around 70% of oral medications are weak bases. And about 25-50% of the top 200 prescribed drugs in the U.S. fall into this category. That means a huge number of people are at risk.
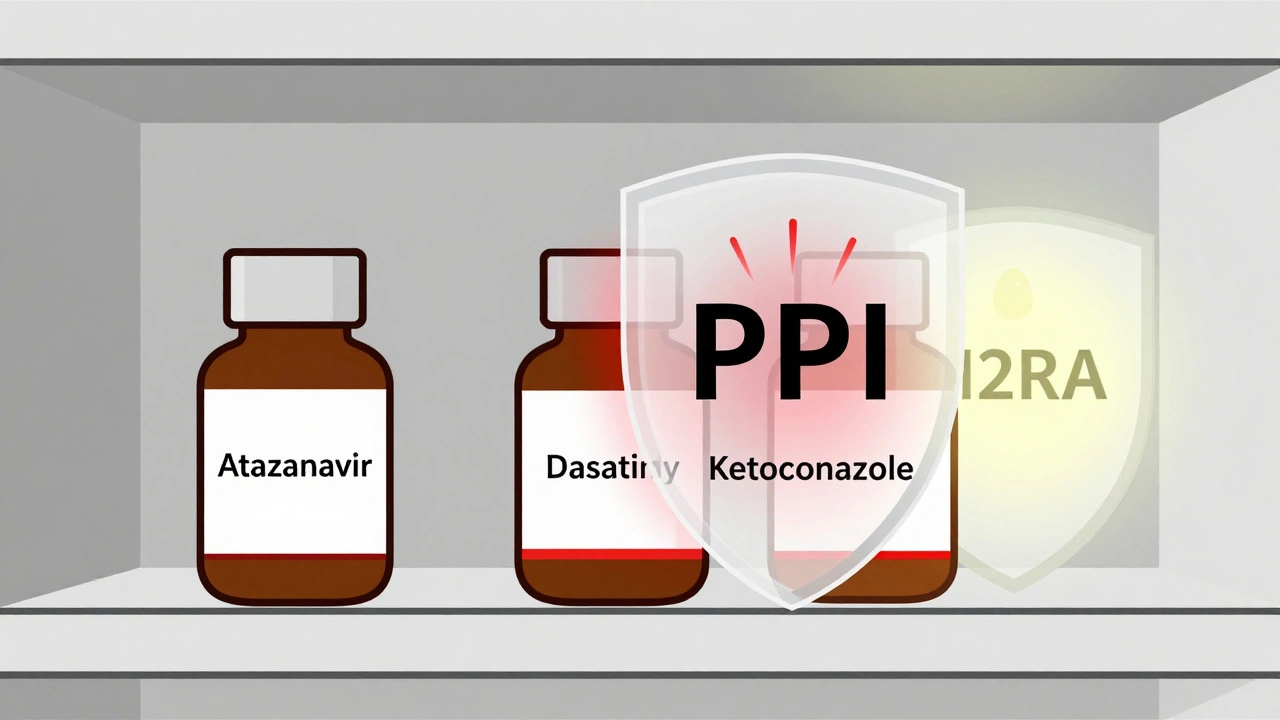
High-Risk Drugs That Lose Effectiveness
Some drugs are hit harder than others. The most dangerous interactions involve drugs with a narrow therapeutic index-where even a small drop in blood levels can cause treatment to fail.
- Atazanavir (an HIV medication): When taken with a PPI, its absorption drops by 74-95%. One patient on Reddit reported their viral load jumped from undetectable to 12,000 copies/mL after starting omeprazole. Their infectious disease doctor confirmed it was a textbook interaction.
- Dasatinib (a leukemia drug): Absorption falls by about 60%. A 2023 study of over 12,000 patients found those on PPIs had 37% higher rates of treatment failure.
- Ketoconazole (an antifungal): This drug becomes nearly useless with PPIs. Studies show a 75% drop in absorption-so much so that doctors now avoid prescribing it with acid reducers entirely.
- Nilotinib and erlotinib: Both cancer drugs show significant absorption drops, requiring dose adjustments or timing changes.
Even drugs you wouldn’t expect are affected. Some blood pressure medications, antifungals, and even certain antidepressants have documented interactions. The FDA has flagged 12 high-risk drugs that now carry explicit warnings about PPI use.
PPIs vs. H2RAs: Not All Acid Reducers Are Equal
Not all acid-reducing drugs are created equal when it comes to interactions. PPIs are far more disruptive than H2RAs.
A 2024 study in JAMA Network Open found that PPIs reduce absorption of pH-dependent drugs by 40-80%. H2RAs, on the other hand, cause a 20-40% reduction. Why? Because PPIs maintain a high pH for much longer-up to 18 hours a day. H2RAs wear off faster, giving the stomach time to return to normal acidity.
That’s why switching from a PPI to famotidine might be a safer option for patients who need both an acid reducer and a high-risk medication. But even H2RAs aren’t risk-free.
Enteric-Coated Pills: A Hidden Danger
Some drugs are designed to dissolve only in the small intestine, not the stomach. These are called enteric-coated tablets. They rely on stomach acid to stay intact until they pass into the duodenum.
When you take a PPI, the stomach becomes less acidic. That can cause these coatings to break down too early-inside the stomach. The drug then gets destroyed by stomach enzymes or causes irritation. This is a silent problem: patients think they’re taking their pill correctly, but the drug never reaches the right spot.
Drugs like esomeprazole itself are enteric-coated. But so are others, like clopidogrel and mesalamine. If the coating dissolves early, the drug’s effectiveness plummets.
What About Acidic Drugs?
Not all drugs are affected the same way. Weakly acidic drugs like aspirin (pKa 3.5) or atenolol actually dissolve better in higher pH environments. But the effect is usually small-only a 15-25% increase in absorption-and rarely clinically significant.
One exception is dasiglucagon, a newer drug for low blood sugar. It shows slightly increased absorption with ARAs, but not enough to require dose changes. For most acidic drugs, the risk is minimal.
Real-World Consequences
This isn’t theoretical. The FDA’s adverse event database recorded over 1,200 reports of therapeutic failure linked to acid-reducing medications between 2020 and 2023. The most common culprits: atazanavir, dasatinib, and ketoconazole.
One patient on Drugs.com wrote: “My doctor didn’t tell me Nexium would interfere with my blood pressure meds-my readings were consistently 20 points higher until we figured out the interaction.”
Another case: a woman with chronic myeloid leukemia was told to take dasatinib with a PPI for GERD. Her cancer progressed. Only after switching to a different acid reducer and staggering the doses did her treatment work again.
These aren’t isolated incidents. A 2023 study estimated that inappropriate PPI use contributes to 15,000-20,000 preventable treatment failures in the U.S. each year.

How to Protect Yourself
If you’re on an acid-reducing medication and take other prescriptions, here’s what to do:
- Ask your pharmacist or doctor: “Could my acid reducer interfere with any of my other meds?” Don’t assume they know. Many providers overlook this.
- Check your pills: Look up your medications on Drugs.com or Medscape. Search for “drug interactions” with your PPI or H2RA.
- Ask about timing: For some drugs, taking them 2 hours before the acid reducer can help. This doesn’t fix everything, but it reduces the risk by 30-40%.
- Consider alternatives: Antacids like Tums or Maalox can be used occasionally with a 2-4 hour gap. But they don’t last long. For long-term use, switching from a PPI to an H2RA might be safer.
- Ask if you really need it: The American College of Gastroenterology says 30-50% of long-term PPI users don’t have a valid reason to be on them. If you’ve been taking omeprazole for years for “heartburn,” ask if you can taper off.
What’s Changing in the Industry
Pharmaceutical companies are finally paying attention. New drugs in development are being designed to work regardless of stomach pH. About 37% of new molecular entities now include special coatings or delivery systems to avoid this problem.
Electronic health records now flag dangerous combinations. Epic Systems reported that 78% of doctors follow alerts when a PPI is prescribed with atazanavir or dasatinib.
Pharmacists are playing a bigger role. A 2023 study showed pharmacist-led reviews cut inappropriate ARA co-prescribing by 62% in Medicare patients.
The FDA now requires companies to test new drugs for pH-dependent absorption issues. They’ve updated guidelines to focus on weak bases with solubility under 0.1 mg/mL at pH above 5-the real danger zone.
What You Can Do Today
You don’t need to be a doctor to protect yourself. If you’re taking any prescription medication and also use an acid reducer, talk to someone who knows the details. Your pharmacist is your best ally. They see all your meds at once. They know the interactions. They can tell you if your heartburn pill is quietly making your other drugs useless.
And if you’ve been on a PPI for years without a clear diagnosis-ask if you can stop. Many people take them long after they’re needed. Reducing or eliminating unnecessary acid reducers doesn’t just prevent interactions-it saves money, reduces side effects, and improves overall health.
This isn’t about fear. It’s about awareness. Your stomach isn’t just a place where food breaks down. It’s a gatekeeper for your entire medication regimen. And if you change its environment, you change how every pill you swallow works.
Can acid-reducing medications make my other drugs less effective?
Yes. Proton pump inhibitors (PPIs) and H2 blockers like omeprazole or famotidine raise stomach pH, which can prevent certain medications from dissolving properly. This is especially true for weakly basic drugs like atazanavir, dasatinib, and ketoconazole. Studies show absorption can drop by 60-95%, leading to treatment failure.
Which acid reducer is safest to use with other medications?
H2-receptor antagonists like famotidine or ranitidine are generally safer than PPIs because they cause less prolonged pH elevation. PPIs keep the stomach pH high for up to 18 hours daily, while H2RAs typically last 8-12 hours. For patients needing long-term acid control, switching from a PPI to an H2RA may reduce interaction risks.
How can I tell if my medication is affected?
Check your medication’s prescribing information for warnings about acid-reducing agents. Drugs with a narrow therapeutic index-like cancer meds, HIV treatments, or antifungals-are most at risk. If you notice your condition worsening after starting an acid reducer (e.g., higher blood pressure, viral rebound, unexplained fatigue), talk to your doctor about a possible interaction.
Should I stop taking my acid reducer?
Don’t stop without talking to your doctor. But do ask whether you still need it. Up to half of long-term PPI users don’t have a valid medical reason to continue. If you’re taking it for occasional heartburn, antacids or lifestyle changes may be enough. Stopping unnecessary PPIs reduces interaction risks and side effects like bone loss and nutrient deficiencies.
Can I take my medications at different times to avoid interactions?
Yes, for some drugs. Taking a weak base medication (like dasatinib) at least 2 hours before your PPI can reduce the interaction by 30-40%. But this doesn’t eliminate the risk. For high-risk drugs like atazanavir, timing isn’t enough-concurrent use is strictly avoided. Always check with your pharmacist before changing your schedule.
ian septian
This is wild. I was on omeprazole for years and never knew it was messing with my blood pressure med. My docs never mentioned it either. Thanks for the heads-up.
Chris Marel
I’m really glad someone laid this out so clearly. I’ve got a friend on HIV meds and they started taking omeprazole for ‘just a little heartburn’-now they’re worried. This post could literally save lives.
Evelyn Pastrana
So let me get this straight… we’re all taking ‘little heartburn pills’ like they’re candy, and somehow that’s quietly sabotaging our cancer drugs? 😅
Thanks for the sarcasm, medicine. Real helpful.
Nikhil Pattni
Guys, this isn’t even the half of it. I’m a pharmacist in Delhi and I’ve seen this happen 30+ times. PPIs mess with absorption of so many drugs-antifungals, antivirals, even some SSRIs. The Henderson-Hasselbalch equation? Yeah, it’s real. But most doctors don’t even know it by name. They just see ‘heartburn’ and write a script. I had a patient on clopidogrel and omeprazole-she had a stroke. Turned out the PPI blocked the activation of clopidogrel. The FDA warned about this in 2009. Still happening. Why? Because nobody checks. Even the EHR alerts get ignored. And don’t get me started on enteric coatings dissolving early-like taking a time-release pill and chewing it. It’s a disaster waiting to happen. And no, switching to famotidine doesn’t fix everything. It just makes it 30% less likely to kill you. Still risky. You need to space doses. 2 hours before. But even then, if you’re on dasatinib? Just don’t. Period. I’ve seen too many patients lose their remission because their GI doc didn’t talk to their oncologist. We need better communication. And yes, I’m ranting. Because people die from this.
Arun Kumar Raut
Big thanks for sharing this. I’ve been on a PPI for years for acid reflux and didn’t realize it could affect my other meds. I’m going to talk to my pharmacist this week. Maybe I can switch to something safer. No need to take more than we need.
precious amzy
How quaint. You reduce gastric acidity, and suddenly the pharmaceutical-industrial complex is in crisis. One must wonder: is the body’s homeostatic equilibrium not sufficient to adapt to the pharmacological interventions we impose upon it? Or is this merely another symptom of our pathological obsession with chemical control over biological processes? The stomach is not a reactor vessel. It is a sacred, ancient, evolutionary mechanism. To presume we can manipulate its pH without consequence is not science-it is hubris dressed in white coats.
iswarya bala
omg i had no idea!! i take nexium and my antidep and now i feel so dumb 😭 i gotta call my doc tmrw
Simran Chettiar
It is worth contemplating the ontological implications of pharmaceutical pH manipulation. The human gastrointestinal tract, as a biophysical interface between the external and internal worlds, has been rendered into a chemically engineered domain. The very act of reducing acidity is not merely a therapeutic intervention-it is an epistemological rupture. We no longer consume drugs; we negotiate with them under altered physiological conditions. The dissolution of the pill is no longer a physiological event but a metaphysical negotiation between molecular structure and pH-dependent solubility. The tragedy lies not in the interaction, but in our collective ignorance of the metaphysics of absorption.
Anna Roh
Wow. So… I’ve been on this stuff for 5 years. I guess I’m just lucky?
Katherine Chan
THIS IS SO IMPORTANT I CANT BELIEVE NO ONE TELLS YOU THIS
talk to your pharmacist they know way more than your doctor sometimes
and if you feel weird after starting a new pill or acid reducer-don’t ignore it
you’re not crazy it’s probably the med
you got this 💪
Philippa Barraclough
While the empirical data presented here is compelling, one must consider the confounding variables inherent in observational studies of drug interactions. The temporal association between PPI administration and therapeutic failure does not necessarily imply causation. Were serum concentrations of the affected drugs measured? Were patient adherence rates controlled for? Were concomitant medications accounted for? The anecdotal reports on Drugs.com and Reddit, while emotionally resonant, lack the rigor of randomized controlled trials. Until we have pharmacokinetic data from prospective studies, we risk overestimating the clinical significance of this interaction.
Tim Tinh
Man, I just found out my cousin’s on dasatinib and was taking omeprazole… she’s been feeling awful. I’m sending her this post right now. Thanks for writing this-so many people are flying blind. Also, typo: ‘famotidine’ not ‘famotodine’ 😅