High blood pressure doesn’t come with warning signs. You might feel fine, but if your numbers are consistently above 130/80, you’re at risk for heart attack, stroke, or kidney damage. That’s why millions of people take blood pressure medications every day - not because they feel sick, but because they need to stay healthy. The right medicine can cut your risk of serious problems by half. But not all pills work the same, and not all side effects are harmless. Knowing the differences between types, what to watch for, and how to stay safe can make all the difference.
How Blood Pressure Medications Work
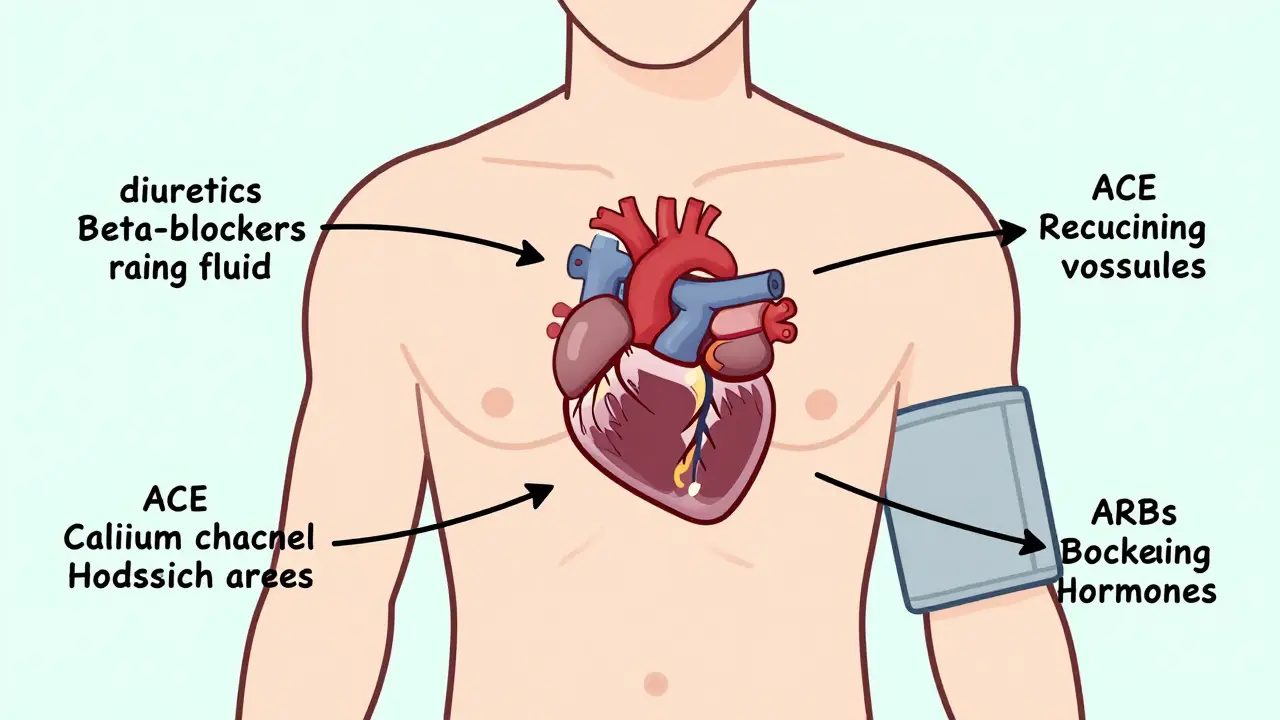
Blood pressure meds don’t just lower numbers - they target how your body controls blood flow. Your heart pumps blood through arteries, and pressure builds when those vessels narrow or your blood volume increases. Different drugs fix different parts of that system.Diuretics, like hydrochlorothiazide, help your kidneys flush out extra salt and water. Less fluid means less pressure on artery walls. Beta-blockers like metoprolol slow your heart rate and reduce how hard your heart pumps. ACE inhibitors such as lisinopril block a hormone that tightens blood vessels, letting them relax. ARBs like losartan do something similar but block the hormone at a different point - which is why they rarely cause the dry cough that plagues ACE users.
Calcium channel blockers, including amlodipine, stop calcium from entering muscle cells in your arteries. That makes the vessels wider and reduces resistance. Alpha-blockers like doxazosin relax artery muscles by blocking nerve signals that tell them to squeeze. Some meds, like methyldopa and clonidine, work in your brain to calm the nervous system’s pressure-boosting signals.
There’s no one-size-fits-all. Your doctor picks based on your age, race, other health issues, and even how your body tends to react to certain drugs. For example, Black patients often respond better to diuretics or calcium channel blockers than ACE inhibitors. If you have diabetes or kidney disease, ACE inhibitors or ARBs are preferred because they protect your kidneys, not just your heart.
The Five Main Classes of Blood Pressure Meds
Most prescriptions fall into five main categories. Each has strengths, weaknesses, and specific uses.
- Thiazide diuretics - Hydrochlorothiazide and chlorthalidone are the most common. They’re cheap, effective, and backed by decades of research. Often the first choice for new patients. Side effects include low potassium, frequent urination, and sometimes gout flare-ups.
- Calcium channel blockers - Amlodipine (Norvasc) is the most prescribed. It’s great for older adults and people with angina. Dihydropyridines like amlodipine mainly relax arteries. Non-dihydropyridines like verapamil also slow heart rate. Common side effects: swollen ankles, dizziness, flushing, and constipation (especially with verapamil).
- ACE inhibitors - Lisinopril, enalapril, and ramipril are widely used. They’re ideal for people with heart failure, diabetes, or kidney disease. The big downside? A persistent dry cough in 10-20% of users. Rare but serious: angioedema (swelling of the face or throat).
- ARBs - Losartan, valsartan, and irbesartan work like ACE inhibitors but without the cough. They’re often used when ACE inhibitors aren’t tolerated. Same risks: high potassium, kidney issues in people with narrowed kidney arteries, and danger in pregnancy.
- Beta-blockers - Metoprolol, atenolol, and carvedilol reduce heart rate and force. They’re not first-line for most people anymore - but they’re essential after a heart attack or for those with heart failure. Side effects: fatigue, cold hands and feet, sleep problems, and they can hide low blood sugar symptoms in diabetics.
Other classes exist - like aldosterone blockers (spironolactone) for resistant hypertension, or vasodilators (hydralazine) for severe cases - but these five cover 90% of prescriptions.
Common Side Effects and What to Do About Them
Side effects are why so many people stop taking their meds. Studies show nearly half quit within a year. But not all side effects mean you need to stop. Some fade. Others can be managed.
Swelling in the ankles from amlodipine? Try elevating your legs, wearing compression socks, or switching to a different calcium blocker. The dry cough from lisinopril? It’s not dangerous - but it’s annoying. Ask your doctor about switching to an ARB like losartan. That cough usually disappears within days.
Diuretics can drain your potassium. Eating bananas, spinach, or sweet potatoes helps. But if you’re on an ACE inhibitor or ARB too, your potassium might go too high instead. That’s dangerous - it can cause irregular heartbeats. Your doctor will check your blood levels every few months.
Beta-blockers can make you feel tired or depressed. Don’t just quit. Talk to your doctor. Maybe your dose is too high, or you need a different beta-blocker. Carvedilol, for example, is less likely to cause fatigue than atenolol.
Orthostatic hypotension - feeling dizzy when you stand up - is common with alpha-blockers and some other meds. Get up slowly. Drink water before standing. Avoid alcohol. If it keeps happening, your dose may need adjusting.
And never ignore swelling in your face, lips, or tongue. That’s angioedema - a medical emergency. Stop the medicine and call 911.
When Medications Are Dangerous Together
Combining blood pressure drugs can be powerful - but risky. Some mixtures are fine. Others can hurt you.
Never take an ACE inhibitor and an ARB together. That doubles your risk of kidney failure and dangerously high potassium. It doesn’t give better protection - only more danger.
NSAIDs like ibuprofen or naproxen can cancel out your blood pressure meds and damage your kidneys. If you need pain relief, acetaminophen (Tylenol) is safer. But even that isn’t risk-free if you’re on diuretics.
Some supplements interfere too. Licorice root can raise blood pressure. St. John’s wort can lower the effectiveness of some meds. Always tell your doctor what you’re taking - even herbal teas or vitamins.
And if you’re pregnant, most blood pressure drugs are off-limits. ACE inhibitors, ARBs, and direct renin inhibitors can cause birth defects. Methyldopa and labetalol are the go-to choices during pregnancy. If you’re planning to get pregnant, talk to your doctor now - don’t wait.
Who Needs More Than One Pill?
Most people don’t get their blood pressure under control with just one drug. About 70% need two or more. The 2025 American Heart Association guidelines say if your blood pressure is above 140/90, start with two meds right away.
Combination pills are common now. You might get a pill that has amlodipine and lisinopril in one tablet. Or hydrochlorothiazide with losartan. That makes it easier to remember. Fewer pills. Fewer chances to skip.
Doctors usually start with one first-line drug. If after four weeks your pressure is still high, they add a second from a different class. Diuretics + calcium channel blockers. ACE inhibitor + diuretic. These pairings work well because they target different systems.
Some people need three or four drugs. That’s not failure - it’s normal. Resistant hypertension isn’t rare. It just means you need a more tailored plan.

Staying Safe and Sticking With Your Treatment
The biggest threat to your health isn’t the medicine - it’s stopping it.
High blood pressure is silent. You won’t feel better when you start taking it. That makes it easy to think, “I don’t need this.” But the damage is still happening. Your arteries are still stiffening. Your heart is still working too hard.
Use a pill organizer. Set phone alarms. Link taking your meds to something you do every day - brushing your teeth, eating breakfast. Apps that track your blood pressure and remind you to take pills can improve adherence by 15-20%.
Keep a log. Write down your readings and any side effects. Bring it to every appointment. That helps your doctor adjust things faster.
Don’t assume a new prescription means you’re cured. Blood pressure control is lifelong. Even if your numbers are perfect, keep taking your pills. Stopping suddenly can cause dangerous spikes.
And if you’re worried about cost - ask. Many generics cost under $5 a month. Some drug companies offer free programs. Your pharmacist can help.
What’s Next for Blood Pressure Treatment?
Science is moving fast. New drugs are being tested for people who don’t respond to current options. Researchers are studying how your genes affect which meds work best. In the next 5-10 years, we may see blood pressure treatment tailored to your DNA.
Wearable tech is helping too. Smartwatches that track blood pressure and sync with apps let you monitor trends at home. That gives doctors more data than a single reading at a clinic.
But the core hasn’t changed. The best medicine is the one you take. The safest choice is the one that fits your life - not just your numbers.
Can I stop taking blood pressure medication if my numbers are normal?
No. Normal numbers mean the medication is working - not that you’re cured. Stopping suddenly can cause your blood pressure to spike, increasing your risk of stroke or heart attack. Some people can reduce or stop meds after major lifestyle changes (weight loss, low-sodium diet, regular exercise), but only under a doctor’s supervision. Never quit on your own.
Which blood pressure medication has the least side effects?
There’s no single answer. Thiazide diuretics like hydrochlorothiazide are generally well-tolerated and have decades of safety data. Calcium channel blockers like amlodipine are also widely used with mild side effects for most people. But side effects depend on the individual. One person’s tolerable side effect is another’s deal-breaker. The best choice is the one that works for your body, health history, and lifestyle - not the one with the fewest side effects on paper.
Why do ACE inhibitors cause a dry cough?
ACE inhibitors block an enzyme that breaks down bradykinin, a substance that can irritate the airways. When bradykinin builds up, it triggers a persistent, tickly cough in about 10-20% of users. It’s not dangerous, but it can be disruptive. Switching to an ARB like losartan usually fixes the cough because ARBs don’t affect bradykinin the same way.
Are natural remedies safe to use with blood pressure meds?
Some can be dangerous. Licorice root raises blood pressure. Garlic and hibiscus tea may lower it too much when combined with meds, causing dizziness or fainting. St. John’s wort can interfere with how your body processes many blood pressure drugs. Always tell your doctor about supplements - even if you think they’re harmless. Natural doesn’t mean safe when mixed with prescription medicine.
How often should I get my blood tested while on these meds?
If you’re on a diuretic, ACE inhibitor, ARB, or aldosterone blocker, your doctor will check your potassium and kidney function within 1-2 weeks after starting or changing the dose, then every 3-6 months if stable. Beta-blockers and calcium channel blockers usually don’t require frequent blood tests unless you have other health issues. Always follow your provider’s schedule - even if you feel fine.
Can I drink alcohol while taking blood pressure medication?
Moderate alcohol (one drink per day for women, two for men) is usually okay, but it can lower blood pressure too much, especially when combined with meds. This increases dizziness and fall risk. Alcohol also interferes with the effectiveness of some drugs and can worsen side effects like drowsiness or dizziness. If you drink, do it slowly and monitor how you feel. Better yet - talk to your doctor about your habits.
David Chase
THIS IS WHY AMERICA IS SICK!!! 😤💊 People are on FIVE different BP meds just because they won’t eat real food or walk 10 minutes a day!! I’ve seen it-my cousin’s on lisinopril, amlodipine, hydrochlorothiazide, carvedilol, AND spironolactone… and he eats McDonald’s for breakfast!! 🍔💀 Stop blaming the pills and start blaming the laziness!! #AmericaFails
Henriette Barrows
I was so scared to start my meds after reading all the side effects… but my doctor said if I didn’t, I’d be at risk for a stroke by 50. I’m on losartan and it’s been 8 months-no cough, no dizziness, just me feeling like I can breathe again. 🙏 You’re not weak for taking pills. You’re smart.
Kevin Lopez
ACEi-induced cough is a class effect mediated by bradykinin accumulation due to ACE inhibition of kininase II. ARBs bypass this pathway via AT1 receptor antagonism. Efficacy equivalence established in multiple RCTs. Diuretics remain first-line per JNC8 for non-black populations. End.
Sharleen Luciano
Honestly, it’s embarrassing how many people treat hypertension like a lifestyle choice rather than a chronic pathophysiological condition. You don’t ‘choose’ to have insulin resistance or endothelial dysfunction. If you’re on meds, you’re not failing-you’re just not doing the research. Most of these comments read like Reddit therapy sessions for people who refuse to read a single peer-reviewed paper.
Duncan Careless
i took my bp med this morning. forgot to write it down. hope my doc doesnt think i skipped it again. 🤷♂️
Tamar Dunlop
I come from a family where hypertension was silent until it wasn’t-my grandmother lost her vision, my uncle had a stroke at 52. I was terrified of the pills… but now, after two years on amlodipine, I walk three miles every morning. I don’t feel ‘fixed’-I feel *protected*. And for that, I am endlessly grateful to modern medicine. 🇨🇦 With deep respect, Tamar
Jim Rice
You all are ignoring the real issue: Big Pharma is pushing these drugs because they make billions. Diuretics cost $3 a month. Why are you on five drugs? Because they want you dependent. Wake up.
Emma Duquemin
Okay, but let’s talk about the *real* MVP here: the humble potassium-rich banana. 🍌 I used to get leg cramps from my diuretic-then I started eating a banana every night with my meds. No more cramps. No more panic. And yes, I also drink hibiscus tea (yes, I know, I told my doctor). It’s not magic-it’s just listening to your body. You don’t need to be a scientist to be smart about your health. Just be consistent. And maybe eat more veggies. 💚
Lisa Dore
I just want to say thank you to everyone who shared their stories. I’ve been on meds for 5 years and I’ve felt so alone. Reading this made me feel seen. You’re not broken. You’re surviving. And that’s enough.