Antidepressant Sweating Risk Calculator
Check Your Medication Risk
When you start an antidepressant to finally feel like yourself again, the last thing you expect is to be drenched in sweat by noon. Yet for one in ten people taking these medications, that’s exactly what happens. This isn’t just uncomfortable-it’s disruptive, embarrassing, and sometimes enough to make someone quit their treatment entirely.
Antidepressant-induced excessive sweating, or ADIES, is real, common, and often misunderstood. It’s not just "being hot" or "nervous." It’s a biological side effect tied to how these drugs interact with your nervous system. You might wake up soaked through your pajamas, need to change shirts three times at work, or avoid social events because you’re terrified of sweating through your clothes. And here’s the catch: this doesn’t always go away with time. Many people live with it for months or even years.
Why Do Antidepressants Make You Sweat So Much?
The answer lies in serotonin. Most antidepressants-especially SSRIs like sertraline, paroxetine, and escitalopram-boost serotonin levels in your brain. That’s good for mood. But serotonin also affects your hypothalamus, the part of your brain that controls body temperature. When this system gets overstimulated, your body thinks it’s overheating… even when it’s not.
It’s not just SSRIs. SNRIs like venlafaxine and even bupropion can trigger sweating. Tricyclic antidepressants, though used less now, are notorious for it. Even if you’ve been on the same medication for months without issue, sweating can suddenly appear. No warning. No pattern. Just one day, you’re soaked.
What makes it worse? This isn’t dose-dependent. Taking a higher dose doesn’t always mean more sweat. Some people on low doses sweat heavily. Others on high doses don’t sweat at all. That’s why simply lowering the dose often doesn’t help.
Which Medications Cause the Most Sweating?
Not all antidepressants are equal when it comes to sweating. Some carry a much higher risk. Here’s what the data shows:
| Medication | Class | Estimated Sweating Incidence | Notes |
|---|---|---|---|
| Paroxetine | SSRI | 19% | Highest risk of all SSRIs |
| Sertraline | SSRI | 15% | Commonly prescribed, high sweating rate |
| Escitalopram | SSRI | 14% | Often causes night sweats |
| Fluoxetine | SSRI | 7% | Lower risk among SSRIs |
| Venlafaxine | SNRI | 13% | Immediate-release form worse than XR |
| Bupropion | NDRI | 11% | Less sexual side effects, but still causes sweat |
| Trazodone | SARI | 5% | Lower risk, often used as alternative |
| Fluvoxamine | SSRI | 4% | Lowest sweating risk among SSRIs |
One surprising finding? Switching from escitalopram to citalopram-even at the same dose-can stop sweating completely. That’s because they’re chemically similar but not identical. The body responds differently to each form. For some, this switch is the difference between continuing treatment and quitting it.
How Bad Is It Really? Real-Life Impact
It’s easy to think, "It’s just sweat." But for those living with it, the consequences are deep.
On Reddit, users share stories like: "I had to change my shirt three times at my job. My boss noticed. I quit." Or: "I stopped taking Paxil after two months. My anxiety improved, but I couldn’t sleep because I was soaked every night. I chose my rest over my mood."
GoodRx reviews show that 68% of people who stopped their antidepressant did so because of sweating. That’s not just discomfort. That’s a treatment failure.
It affects sleep, work, relationships, and self-esteem. Imagine wearing a dark shirt to a job interview and seeing sweat stains bloom under your arms. Or having your partner wake up to your soaked pillow and ask, "Are you okay?" You start avoiding hugs, dates, even showers-because you’re afraid of what comes next.
This isn’t a minor annoyance. It’s a quality-of-life issue that deserves real attention.

What You Can Do: Cooling Strategies That Actually Work
There’s no one-size-fits-all fix, but there are proven ways to manage it. Here’s what works, backed by research and real experience.
1. Switch Medications
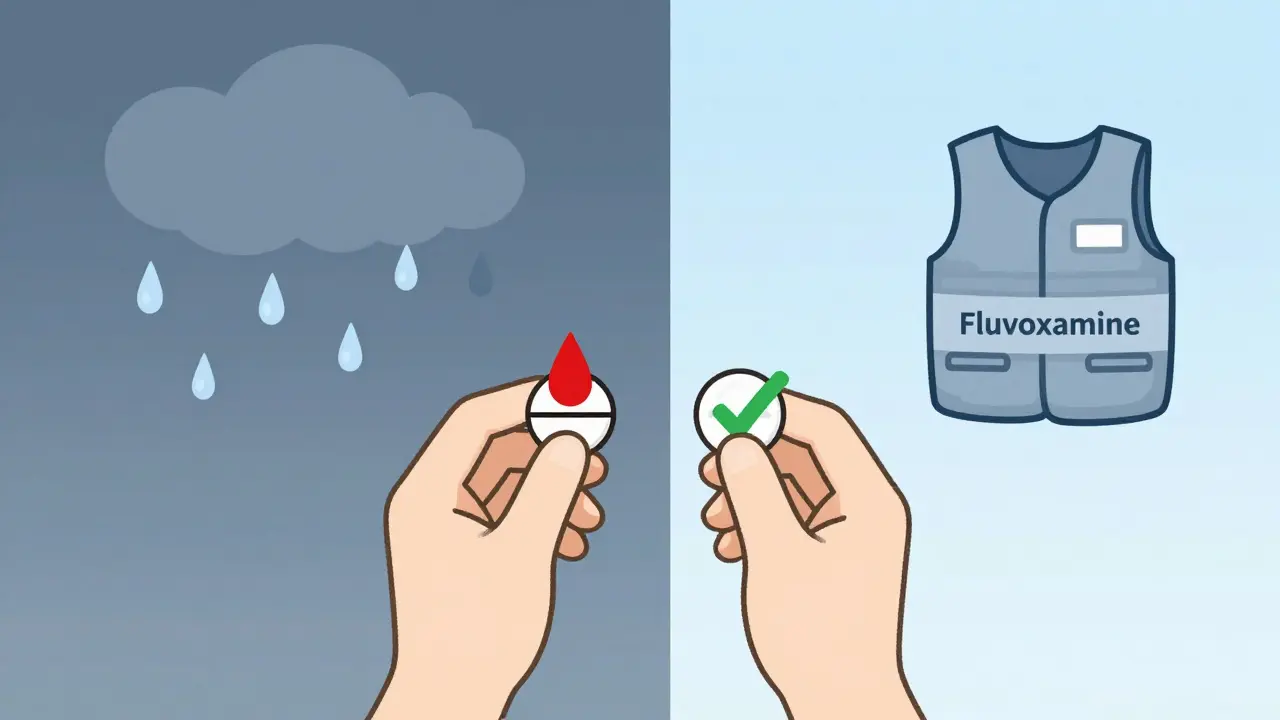
This is often the most effective step. If you’re on paroxetine or sertraline, talk to your doctor about switching to something with lower sweating risk. Fluvoxamine, trazodone, or even citalopram (if you’re on escitalopram) are strong alternatives. Don’t assume your current med is your only option. Many people find relief without losing their mental health gains.
2. Try a Non-Systemic Cooling Vest
A 2022 pilot study tested cooling vests in people with antidepressant-induced sweating. The result? 60% reduction in sweating episodes. These aren’t fancy gym gear-they’re lightweight, wearable vests with gel packs that stay cool for hours. You can wear them under shirts. They’re discreet. And they work.
They’re especially helpful for work, travel, or hot weather. One user in Wellington described wearing hers under her work blazer during summer meetings. "I didn’t feel like a mess. I felt like me again."
3. Use Clinical-Strength Antiperspirants
Regular deodorants won’t cut it. You need antiperspirants with 15-20% aluminum chloride. Apply them at night to dry skin-especially underarms, scalp, and neck. This blocks sweat glands temporarily. It’s not a cure, but it reduces output by 50-70% for many. Reapply every few days.
4. Wear Moisture-Wicking Fabrics
Not all clothes are created equal. Cotton soaks up sweat and clings. Instead, choose technical fabrics designed for athletes: polyester blends, merino wool, or bamboo-based materials. These pull moisture away from your skin and dry fast. Look for labels like "anti-odor," "quick-dry," or "thermoregulating."
5. Consider Adjunct Medications
If switching meds isn’t possible, your doctor might suggest adding a low-dose medication to block the sweating. Two options have strong evidence:
- Glycopyrrolate (1-2 mg daily): An anticholinergic that reduces sweat production. Side effects include dry mouth and constipation, but many tolerate it well.
- Benztropine (0.5-1 mg daily): Often used for Parkinson’s, it also reduces sweating. Less drying than glycopyrrolate, but may cause dizziness.
These aren’t first-line, but they’re life-changing for people who’ve tried everything else.
When to Worry: Sweating vs. Serotonin Syndrome
Not all sweating is harmless. If your sweat is accompanied by:
- Fast heartbeat
- Tremors or muscle stiffness
- Confusion or hallucinations
- High fever
…this could be serotonin syndrome-a rare but dangerous condition. It needs immediate medical attention. Don’t wait. Go to the ER. This is not a "wait and see" situation.
What’s Next? The Future of Managing This Side Effect
Researchers are making real progress. A 2024 tool called the Anticholinergic Risk Scale now rates antidepressants by their sweating risk. Paroxetine scores a 4/4 (highest). Fluvoxamine scores 1/4 (lowest). Doctors are starting to use this to pick safer options.
New delivery methods are coming too. Transdermal patches like selegiline cause 60% less sweating than oral SSRIs. And a new antidepressant in Phase II trials, LS-2-1123, caused sweating in only 3.2% of users-compared to 14.7% with escitalopram.
By 2027, genetic testing might tell you ahead of time if you’re likely to sweat heavily on a certain drug. That could cut the problem in half.
For now, though, you have tools. You have options. You don’t have to suffer in silence.
Frequently Asked Questions
Is excessive sweating from antidepressants normal?
Yes, it’s common-but not inevitable. Between 7% and 22% of people on antidepressants experience it, depending on the drug. It’s not a sign you’re doing something wrong. It’s a biological side effect, like nausea or dry mouth. The key is recognizing it early and addressing it, not just accepting it.
Will I get used to the sweating over time?
Usually not. Unlike nausea or drowsiness, which often fade after a few weeks, excessive sweating from antidepressants typically doesn’t improve with time. Studies show symptoms persist for months or longer. If you’ve been sweating for over six weeks, don’t wait for it to go away-talk to your doctor about solutions.
Can I just stop taking my antidepressant?
No. Stopping abruptly can cause withdrawal symptoms, worsen depression, or trigger rebound anxiety. If sweating is unbearable, work with your doctor to switch medications gradually. Never stop on your own. There are safer alternatives.
Does being overweight make it worse?
Not directly. Sweating from antidepressants is caused by brain chemistry, not body weight. However, excess weight can make you feel hotter and sweat more overall, which might make the problem feel worse. Focus on the medication and cooling strategies first-weight isn’t the root cause.
Are there natural remedies that help?
There’s no strong evidence that herbs, supplements, or acupuncture reduce antidepressant-induced sweating. What does work? Clinical antiperspirants, moisture-wicking clothes, cooling vests, and medication changes. Don’t waste time on unproven fixes. Stick with science-backed methods.
Can I use Botox for this?
Yes, but it’s not usually the first choice. Botox injections block sweat glands in specific areas like underarms. It works well for focal sweating and lasts 4-6 months. But it’s expensive, painful, and doesn’t help with sweating on the scalp or torso. It’s best for people who’ve tried everything else and only sweat in one area.
Should I avoid exercising?
No. Exercise is still important for mental health. Just plan ahead. Wear moisture-wicking clothes, carry a towel, and cool down with a fan or cold water after. Many people find that once they get used to managing the sweat, they can still enjoy workouts. Don’t let this side effect rob you of movement.
Next Steps: What to Do Today
If you’re struggling with this:
- Track your sweating: Note when it happens, how bad it is, and what you’re wearing.
- Check your medication: Look up its sweating risk in the table above.
- Buy a clinical antiperspirant: Get one with 15-20% aluminum chloride.
- Invest in one moisture-wicking shirt: Try it for a week.
- Schedule a talk with your doctor: Ask about switching or adding a low-dose anticholinergic.
You didn’t sign up for this. But you can fix it. You’re not alone. And you don’t have to live in sweat-soaked clothes.

Eric Knobelspiesse
so like... i read this and im just like wow. i been on sertraline for 3 years and yeah i sweat like a damn sauna. never thought it was the med. thought i was just outta shape. turns out its the damn brain chemistry. thanks for the table. now i know why my boss keeps handing me towels at meetings. i might switch to fluvoxamine. or just move to alaska.