Medication Heartburn Risk Calculator
Why Your Medication Is Giving You Heartburn
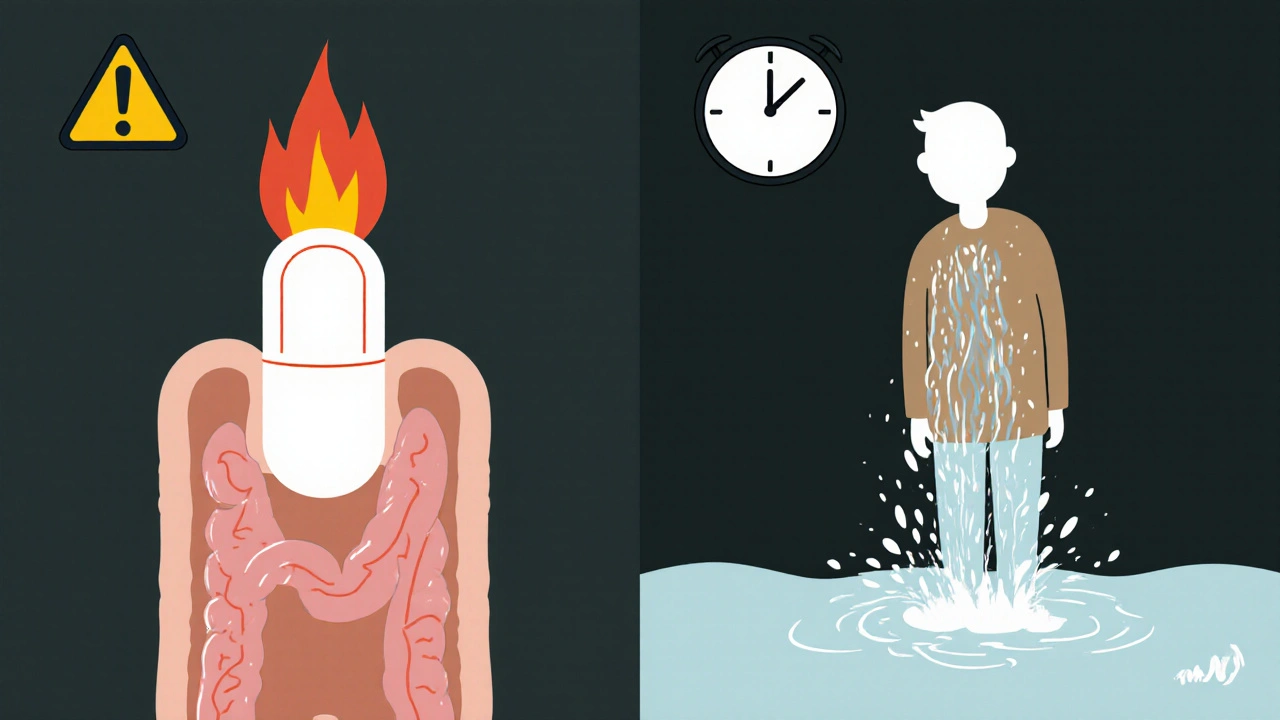
It’s not just spicy food or too much coffee. If you’ve been popping pills and suddenly feel that burning in your chest or a churning in your stomach, your medication might be the real culprit. About 1 in 5 people who take common drugs like ibuprofen, antibiotics, or blood pressure meds end up with heartburn or an upset stomach-not because they’re doing anything wrong, but because the medicine itself is irritating their digestive system.
This isn’t rare. Healthgrades reports that 40% of Americans get heartburn at least once a month, and up to 20% of those cases come from medications, not diet. The problem isn’t always the drug’s purpose-it’s how it interacts with your esophagus and stomach lining. Some drugs weaken the muscle that keeps stomach acid down. Others scratch or burn the tissue directly. And some increase acid production, turning your stomach into a pressure cooker.
Top Medications That Cause Heartburn
Not all pills are created equal when it comes to stomach trouble. Some are far more likely to cause problems than others.
- NSAIDs like ibuprofen and aspirin are the biggest offenders. They block protective chemicals in your stomach lining, leaving it exposed to acid. Up to 30% of people who take ibuprofen regularly get heartburn. Long-term use raises the risk of ulcers from 1-2% to 15-30%.
- Tetracycline antibiotics, especially doxycycline, can cause serious esophagitis if swallowed without enough water or if you lie down right after. About 12% of users get pill-induced burns in their esophagus-sometimes within hours.
- Calcium channel blockers (like amlodipine and nifedipine), used for high blood pressure, relax the lower esophageal sphincter. This lets acid splash up into your throat. Around 10-20% of users report heartburn.
- Theophylline, an asthma drug, weakens the same muscle by 30-50%, leading to reflux in 25-30% of users.
- Metformin, the most common diabetes pill, causes nausea, bloating, and heartburn in 20-30% of new users. The good news? For 60-70% of people, these symptoms fade after 2-4 weeks.
- Bisphosphonates like alendronate (used for osteoporosis) are the most dangerous. If taken incorrectly, they can cause severe ulcers or even require hospitalization. About 5-10% of users develop esophagitis.
How to Take Pills Without Burning Your Throat
Many of these side effects aren’t unavoidable. Simple habits can cut your risk dramatically.
- Drink a full 8-ounce glass of water with every pill. This is especially critical for antibiotics and bone meds. Water washes the pill down before it sits and dissolves in your esophagus. Studies show this reduces esophagitis risk by 60-70%.
- Stay upright for at least 30-60 minutes after taking your medicine. Don’t lie down, bend over, or slump in a chair. Gravity keeps the pill moving and prevents it from sticking. For doxycycline and alendronate, this one step prevents 80-90% of cases of pill-induced injury.
- Take NSAIDs with food. Eating before or with ibuprofen or aspirin reduces stomach irritation by 40-50%. But don’t do this with antibiotics or bisphosphonates-they need an empty stomach to work properly.
- Avoid alcohol and caffeine around medication time. Both relax the esophageal sphincter and increase acid, making heartburn worse.
When to Use Antacids or PPIs
If you’re stuck with a medication that causes heartburn, you don’t have to suffer. Over-the-counter options can help-but they’re not all the same.
- Antacids like Tums or Rolaids give quick relief by neutralizing acid. Taking one 30 minutes before your NSAID can reduce heartburn by 30-40%.
- Proton pump inhibitors (PPIs) like omeprazole or esomeprazole cut acid production for hours. For people on long-term NSAIDs, especially those over 50 or with a history of ulcers, adding a PPI reduces ulcer risk by 70-80%.
- H2 blockers like famotidine (Pepcid) are milder than PPIs but still help. They’re good for occasional heartburn but less effective for daily protection.
Don’t start a PPI without talking to your doctor. Long-term use can have side effects like nutrient deficiencies or increased infection risk. But for many, the benefit of staying on their heart or diabetes meds outweighs the risk.
Red Flags That Mean You Need a Doctor
Most medication-related heartburn is annoying, not dangerous. But some symptoms signal real trouble.
- Chest pain that feels like pressure, tightness, or radiates to your arm or jaw. This could be heart-related, not just acid.
- Difficulty swallowing or feeling like food gets stuck. This suggests inflammation or scarring in the esophagus.
- Blood in vomit or stool (looks like coffee grounds or black, tarry stools). This means bleeding in your stomach or intestines-often from NSAID-induced ulcers.
- Unexplained weight loss or persistent nausea. These could point to ongoing damage or something more serious.
If you have any of these, don’t wait. See your doctor. You might need an endoscopy to check for ulcers or Barrett’s esophagus-a condition where the esophagus lining changes due to chronic acid exposure, increasing cancer risk.

What You Should Never Do
It’s tempting to quit a pill that’s making you feel bad. But stopping without talking to your doctor can be dangerous.
- Don’t stop blood pressure meds like beta blockers or calcium channel blockers on your own. Abruptly stopping can cause spikes in blood pressure, heart attacks, or arrhythmias.
- Don’t skip diabetes meds like metformin just because your stomach feels off. The GI side effects usually fade. Talk to your doctor about switching to a slow-release version if needed.
- Don’t crush or chew pills unless the label says it’s okay. Some are designed to release slowly. Crushing them can cause a flood of drug in your throat or stomach.
- Don’t assume it’s just "indigestion". If you’ve been taking a new drug and the heartburn started shortly after, connect the dots. Tell your doctor exactly when it began and what you’re taking.
Newer Options and Future Fixes
Pharma companies are finally catching up. In 2022, the FDA approved a new delayed-release version of doxycycline that dissolves in the intestine, not the esophagus. This cuts esophagitis risk by half.
New NSAID formulations with protective coatings are in use now and reduce heartburn by 30-35% in trials. Electronic health records now flag patients at risk-like someone on both NSAIDs and a calcium channel blocker-and alert doctors to suggest alternatives.
Future treatments may include genetic tests to spot people who metabolize NSAIDs poorly (15-20% of Caucasians), or patches and sprays that deliver drugs without going through the gut at all. These are still in testing, but they show how seriously the medical world is taking this issue.
Bottom Line: Manage It, Don’t Just Endure It
Medication-induced heartburn isn’t something you have to live with. It’s not a sign you’re weak or doing something wrong. It’s a known side effect with proven solutions.
Start by tracking: What pills are you taking? When did the heartburn start? Does it happen every time, or only when you skip water or lie down?
Then talk to your doctor. Ask: "Is there a gentler alternative?" "Can I take this with food?" "Should I use a PPI while on this?" "Is there a newer version of this drug?"
Most people can keep their essential meds and avoid heartburn-without quitting, without suffering, and without risking long-term damage.
Can I take ibuprofen if I have heartburn?
You can, but it’s risky. Ibuprofen can make heartburn worse and increase your chance of stomach ulcers. If you need pain relief, take it with food and a full glass of water. Consider switching to acetaminophen (Tylenol), which doesn’t irritate the stomach. If you must use ibuprofen long-term, ask your doctor about adding a proton pump inhibitor to protect your lining.
Does metformin cause permanent stomach damage?
No, metformin doesn’t cause permanent damage. About 20-30% of new users get nausea, bloating, or heartburn, but these symptoms usually fade within 2-4 weeks. Switching to the extended-release version can cut side effects by half. If symptoms last longer than a month, talk to your doctor about adjusting your dose or trying a different diabetes medication.
Can doxycycline cause permanent esophagus damage?
Yes, if taken incorrectly. Doxycycline can cause severe burns or ulcers in the esophagus if swallowed without enough water or if you lie down right after. In rare cases, this leads to scarring or narrowing of the esophagus. But 95% of these cases are preventable by taking the pill with a full glass of water and staying upright for at least an hour. New delayed-release versions also reduce this risk dramatically.
Should I stop my blood pressure pill if it gives me heartburn?
Never stop a blood pressure medication without talking to your doctor. Calcium channel blockers like amlodipine can cause heartburn, but stopping them suddenly can cause dangerous spikes in blood pressure. Instead, ask if you can switch to a beta blocker, which causes heartburn in only 5-10% of users. Your doctor may also recommend a PPI or suggest taking the pill earlier in the day to reduce nighttime reflux.
Are natural remedies like ginger or apple cider vinegar safe for medication-induced heartburn?
Ginger may help with nausea from metformin, but it’s not a cure for drug-induced heartburn. Apple cider vinegar is not recommended-it’s acidic and can make reflux worse. Don’t rely on home remedies to treat this. The real fix is adjusting how you take your pills, using proven medications like antacids or PPIs, and talking to your doctor about alternatives. Natural remedies can delay proper care and risk serious damage.

Melanie Taylor
OMG YES THIS!!! 🙌 I was on doxycycline and thought I was dying-burning throat, can't swallow water... turned out I was lying down 5 mins after taking it. Now I stand like a statue for an hour. LIFE CHANGER. 🤯
Rachel Wusowicz
This is all a distraction... Big Pharma doesn't want you to know that stomach acid is actually a *bio-electrical signal*-and these pills? They're tampering with the Earth's natural pH resonance. The water? It's not for washing down-it's to dilute the electromagnetic interference from the pills' coating. They're testing this on us... and you're just drinking it... 🧪💧
Teresa Smith
While the practical advice here is sound-hydration, upright posture, avoiding alcohol-it's critical to recognize that pharmaceutical side effects are not merely biological phenomena, but systemic indicators of a medical model that prioritizes efficacy over holistic tolerance. We must advocate for patient-centered pharmacology, not just symptom management.
David Rooksby
Okay so let me get this straight-you’re telling me that if I just drink water and don’t lie down, I won’t get heartburn from my blood pressure meds? Bro, that’s like saying if you don’t touch a live wire you won’t get electrocuted. DUH. But who the hell remembers to do that every single time? I’m 42, I take 8 pills a day, and I’m not a robot. Also, PPIs? They’re basically chemical sedatives for your stomach. You think your gut’s happy? Nah. It’s just numb. And your microbiome? Gone. Like, poof. Like the whole thing’s been wiped clean by Big Pharma’s little magic potion.
Deepak Mishra
I took metformin and it felt like my stomach was a volcano that just erupted!!😭 I cried in the bathroom for 20 mins... then I switched to ER version and now I’m chill 😎 but my cousin said she took ginger tea and it fixed everything?? I’m confused now 🤯
Dan Angles
The recommendation to take NSAIDs with food is scientifically valid and clinically supported. However, it is imperative to distinguish between the pharmacokinetic implications of food co-administration and the underlying pathophysiology of mucosal injury. A comprehensive risk-benefit analysis, including gastrointestinal bleeding risk stratification via the ABCD2 score, should precede any therapeutic modification.
John Mwalwala
Look, the real issue here is bio-accumulation of proton pump inhibitors. We're not just talking about stomach acid-we're talking about mitochondrial disruption, gut flora collapse, and long-term B12 deficiency cascades. PPIs are the silent killers of the microbiome. And no one's talking about it. The FDA? They're asleep. The pharma reps? They're in your doctor's office right now. You're being sold a solution that creates five new problems.
Diane Tomaszewski
I took ibuprofen with food and drank water and it stopped hurting. I didn't need a PPI. I just listened to my body. Sometimes simple works
ZAK SCHADER
This whole article is a liberal brainwash. Americans are weak. Back in my day, we took pills dry and walked uphill both ways. If your stomach burns, you’re just not tough enough. Stop whining. And why are we trusting some doctor’s blog over real medicine? This isn’t science-it’s wellness influencer nonsense.
Danish dan iwan Adventure
Metformin-induced GI distress is a known pharmacodynamic artifact due to GLUT2 inhibition in enterocytes. Extended-release formulations mitigate this via delayed mucosal exposure. Compliance remains suboptimal. Recommend titration + fiber supplementation. End of discussion.
Ankit Right-hand for this but 2 qty HK 21
You people are so soft. I take my pills without water, lie down immediately, and still run marathons. Your stomach is weak because your mindset is weak. This is why America is falling behind. Stop crying about heartburn and start lifting weights. Also, why are you trusting Western medicine? India has better herbs. You just don't want to try them.
Oyejobi Olufemi
You think this is about stomach acid? No. This is about control. They put these chemicals in your body to make you dependent. Then they sell you PPIs to fix the damage they created. Then they sell you supplements to fix the PPI damage. Then they sell you… you get it. It’s a pyramid. The esophagus? Just the first domino. The real villain? The pharmaceutical-industrial complex. They own your doctor. They own your FDA. They own your sleep. And now you’re reading this… and you’re still taking the pills. 😔
Daniel Stewart
There’s an existential weight to the act of swallowing a pill-each one a silent pact with an invisible system. We ingest not just molecules, but the architecture of modern healthcare: efficiency over empathy, profit over presence. The burning is not merely physiological-it is the echo of our surrender to systems that do not see us as whole beings, but as data points with side effects.