Drug Interaction Risk Calculator
Statins & Antifungals Risk Assessment
This tool helps you understand the risk level of combining specific statins with systemic antifungals based on CYP3A4 inhibition.
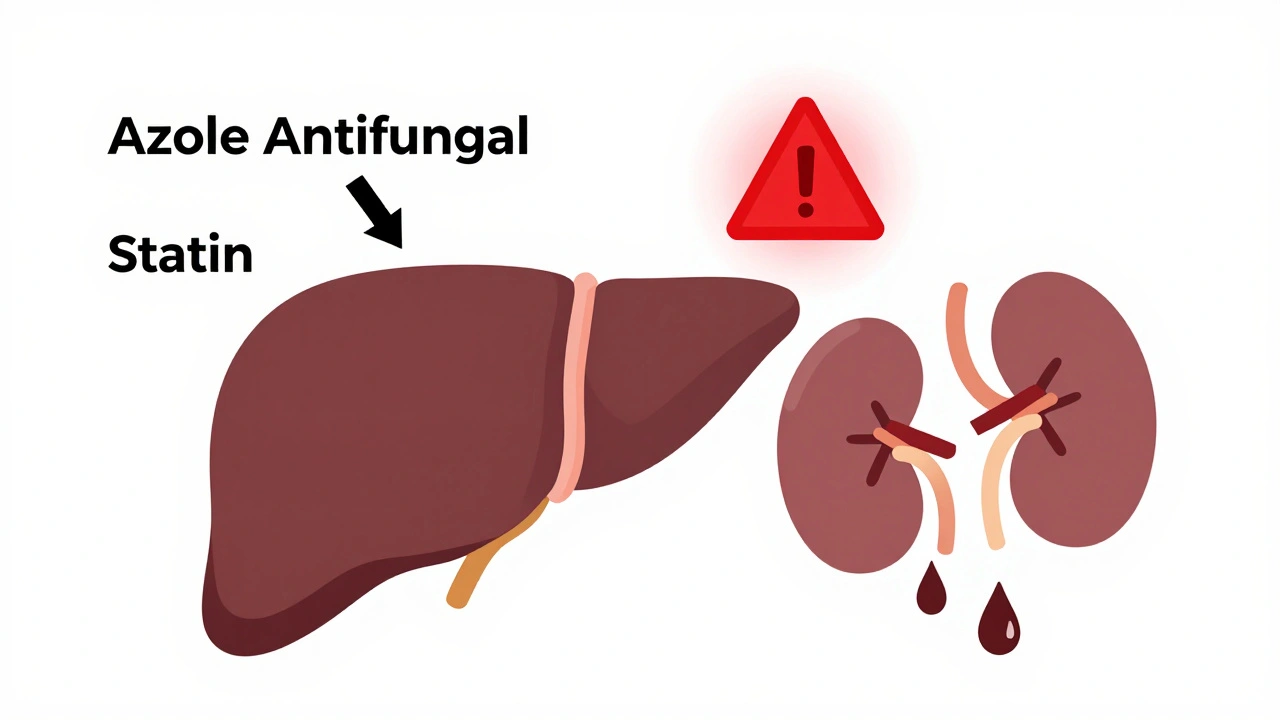
When you're taking a statin to lower your cholesterol and need an antifungal for a stubborn infection, it's not just about popping pills. Some combinations can turn dangerous-fast. Systemic antifungals, especially the azole class, don't just fight fungi. They also mess with how your body processes other drugs, including statins and immunosuppressants. The result? Muscle damage so severe it can lead to kidney failure or death.
Why Azole Antifungals Are So Risky
Azole antifungals like itraconazole, voriconazole, posaconazole, and fluconazole work by blocking a fungal enzyme called lanosterol 14-alpha-demethylase. But here’s the catch: that same enzyme is part of a family in your liver called cytochrome P450, specifically CYP3A4. This enzyme handles the breakdown of more than 30% of all prescription drugs, including most statins and immunosuppressants.When azoles inhibit CYP3A4, they slow down or stop the metabolism of these drugs. That means the statin or immunosuppressant builds up in your bloodstream-sometimes 10 to 20 times higher than normal. This isn't theoretical. Studies show patients on simvastatin and ketoconazole had statin levels spike by 15 to 20 times. That’s not a typo.
Not all azoles are equal. Ketoconazole and posaconazole are the worst offenders. Fluconazole is less potent but still risky, especially at higher doses. Voriconazole and itraconazole also strongly inhibit CYP3A4. Even newer ones like isavuconazole, while better, still need caution. The bottom line: if you're on one of these antifungals, your statin could become a ticking time bomb.
Which Statins Are Most at Risk?
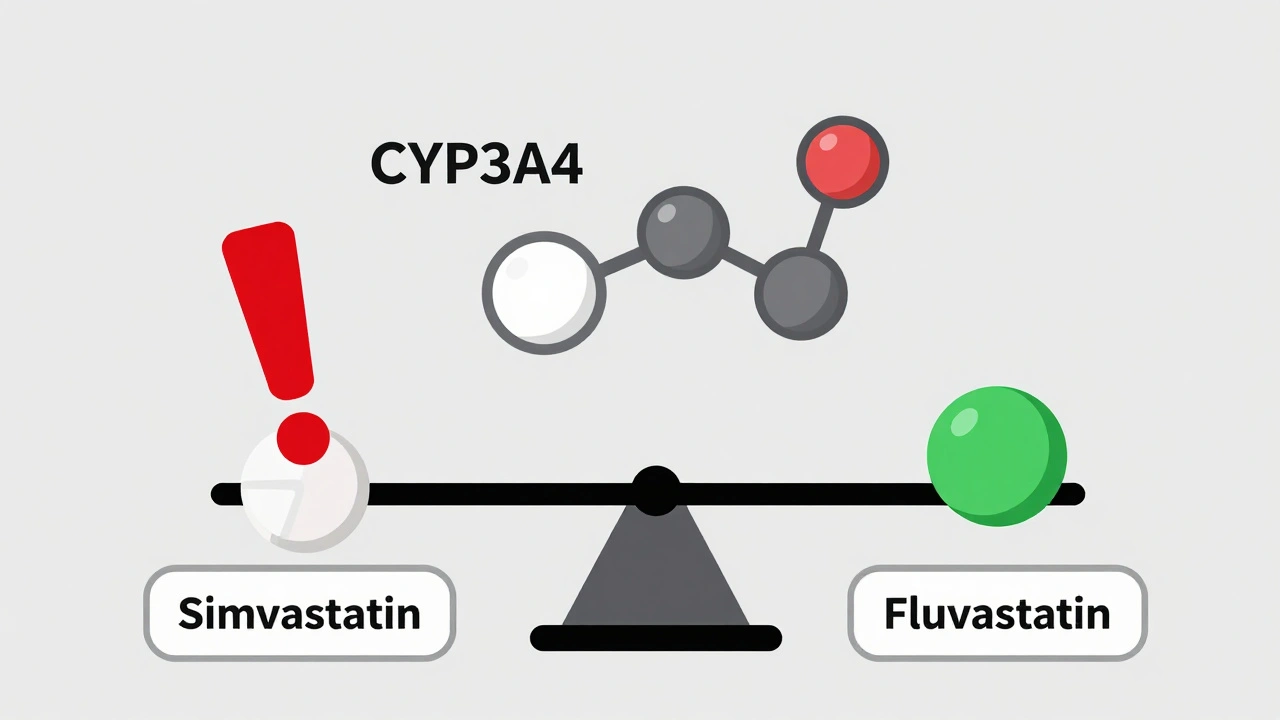
Statins aren’t all the same. Their risk level depends on how they’re processed in your body.- High risk: Atorvastatin, simvastatin, lovastatin. These are metabolized almost entirely by CYP3A4. Taking them with azoles like posaconazole or ketoconazole can push your statin levels into toxic territory.
- Lower risk: Pravastatin and rosuvastatin. These don’t rely much on CYP3A4. But here’s the twist: ketoconazole can still raise their levels by blocking the OATP1B1 transporter, which helps move statins out of the liver. So even these "safer" options aren’t risk-free.
- Minimal risk: Fluvastatin and pitavastatin. These use different metabolic pathways and are often the best choices when antifungals are needed.
Case reports have documented creatine kinase (CK) levels over 10,000 U/L in patients on simvastatin and azoles. Normal CK is under 200 U/L. Levels above 1,000 U/L mean muscle breakdown is happening. Above 5,000 U/L? You’re at high risk of rhabdomyolysis-a condition where muscle tissue dissolves and floods your kidneys with toxic proteins.
Immunosuppressants Make It Worse
If you’ve had a transplant, you’re already on drugs like cyclosporine, tacrolimus, or sirolimus. These are also strong CYP3A4 inhibitors. So now you’ve got two inhibitors: the antifungal and your immunosuppressant-both squeezing the same metabolic pathway.Studies show that when statins are added to cyclosporine, statin levels jump 3 to 20 times higher than normal. In transplant patients, up to 25% develop muscle pain or weakness from statins alone. Add an azole antifungal? That risk multiplies.
One 2019 analysis from the American College of Cardiology found that transplant patients on statins and immunosuppressants had a tenfold increase in rhabdomyolysis risk compared to those on statins alone. And that was before adding antifungals.
The danger isn’t just theoretical. Emergency rooms see these cases every year. Patients come in with severe muscle pain, dark urine, and kidney failure-all because their meds weren’t reviewed properly.
What Should You Do?
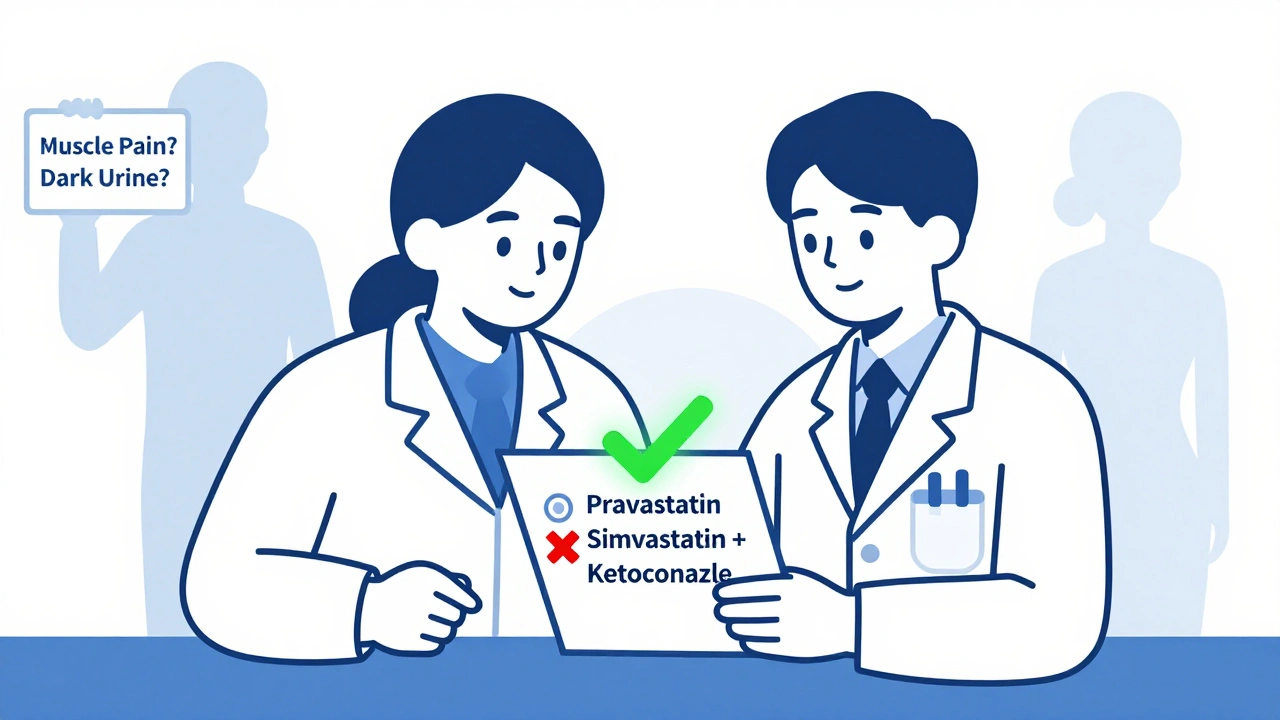
If you're prescribed an azole antifungal and you're on a statin, here’s what needs to happen:- Stop high-risk statins immediately. If you're on simvastatin, lovastatin, or atorvastatin, stop them before starting the antifungal. Don’t wait for symptoms.
- Switch to a safer statin. Use pravastatin (10-40 mg daily) or rosuvastatin (5-20 mg daily). These are the safest options. Fluvastatin or pitavastatin are good alternatives.
- Never exceed 10 mg of simvastatin. Even this low dose is risky with moderate CYP3A4 inhibitors like fluconazole. Avoid it entirely if possible.
- Monitor your muscles. Watch for unexplained muscle pain, weakness, or dark urine. Check CK levels before starting the antifungal and again after 1-2 weeks.
- Wait before restarting. After finishing the antifungal, wait at least 7 days before restarting a statin-longer if you were on posaconazole, which sticks around for 24-30 hours.
For transplant patients, the rules are stricter. Your doctor should monitor your immunosuppressant blood levels closely. When you start an azole, your cyclosporine or tacrolimus dose may need to be cut by 30-50% to avoid toxicity. Your pharmacist should be involved in every step.
Why Do These Interactions Keep Happening?
You’d think doctors would know better. But they don’t always.Statins are among the most prescribed drugs in the world-nearly 39 million Americans take them. Fluconazole alone is prescribed over 5 million times a year in the U.S. That’s a lot of overlap. Even with clear warnings on drug labels, studies from 2012 show these dangerous combinations are still common.
Why? Because prescribing is fast. Doctors are overwhelmed. Electronic health records sometimes don’t flag the risk unless they’re properly configured. Community pharmacies often lack the resources to catch every interaction.
But progress is being made. Academic medical centers that use pharmacist-led drug reviews have cut high-risk combinations by 63%. Electronic alerts that pop up when a doctor tries to prescribe simvastatin with ketoconazole have reduced unsafe prescriptions by 47%.
Still, the problem persists. If you’re on one of these drugs, don’t assume your doctor knows. Ask.
What’s New and Hopeful?
There’s light at the end of the tunnel.New antifungals like olorofim are being tested. Unlike azoles, it doesn’t touch CYP450 enzymes at all. Early trials show it’s effective against resistant fungi-and doesn’t interfere with statins or immunosuppressants. If approved, it could be a game-changer.
Also, pharmacogenomics is starting to help. About 12% of people have a genetic variant in the SLCO1B1 gene. This makes them far more likely to develop muscle damage from statins-even at normal doses. If you’ve had unexplained muscle pain on statins before, ask about genetic testing. It could save your life next time.
And guidelines are tightening. The American Society of Health-System Pharmacists now requires pharmacists to verify all azole prescriptions in 87% of major hospitals. That’s a big step forward.
Bottom Line: Don’t Guess. Ask.
If you’re on a statin and need an antifungal, don’t just take the prescription. Ask:- Is this antifungal a strong CYP3A4 inhibitor?
- Which statin am I on-and is it safe with this drug?
- Should I stop my statin? For how long?
- Do I need a blood test before or after starting?
These interactions aren’t rare. They’re predictable. And they’re deadly. But they’re also preventable.
Know your meds. Speak up. Your muscles-and your kidneys-will thank you.
Annie Grajewski
so like... if i'm on simvastatin and get a yeast infection, do i just suffer through it? or do i become a medical martyr? 🤔 also why does my pharmacist look at me like i'm asking for a bomb manual when i ask about this?
Norene Fulwiler
I've seen this happen to my uncle after his kidney transplant. They gave him fluconazole for a thrush flare-up and he ended up in the ER with muscle so bad he couldn't stand. They didn't even check his statin. He's lucky he didn't lose a leg. This isn't just a 'warning'-it's a ticking clock and half the docs don't even know the alarm's going off.
Harry Nguyen
This is why America's healthcare is a dumpster fire. You need a PhD to take a pill now. Meanwhile, in Germany they just give you a shot and tell you to shut up. We turned medicine into a choose-your-own-adventure novel written by lawyers.
Deborah Jacobs
I remember my grandma-bless her-taking her statin like candy and then getting that fungal toenail thing. The doc handed her fluconazole like it was aspirin. Two weeks later she was hobbling around saying her legs felt like wet concrete. We found out the hard way. Now I keep a little cheat sheet taped to my fridge: 'If it ends in -azole, pause the statin.' Simple. Savvy. Survival.
Kylee Gregory
It’s fascinating how biology doesn’t care about our convenience. The same enzyme that protects us from fungi also keeps our meds from poisoning us. We’re not fighting disease-we’re negotiating with our own biochemistry. Maybe we should stop treating drugs like interchangeable toys and start seeing them as part of a living system. Just a thought.
Lucy Kavanagh
You know who’s really behind this? Big Pharma. They want you dependent on statins so they can sell you more antifungals that interact with them. Then they profit from the ER visits. It’s all calculated. I read on a forum that the FDA gets funding from these companies. They bury the truth. Ask yourself: why are they still selling simvastatin with azoles? Coincidence? Or conspiracy?
Michael Dioso
Let’s be real-most people don’t even know what CYP3A4 is. You think your 62-year-old aunt who takes 7 meds and watches Dr. Oz is reading journal articles? Nah. She’s trusting the script. The system is broken. And no, switching to rosuvastatin isn’t a magic fix. I’ve seen people on 'safe' statins still get rhabdo because their doc didn’t check their other meds. You’re not safe until you’ve got a pharmacist yelling at you.
Krishan Patel
This is precisely why Western medicine is a house of cards. We create complex pharmacological systems, then expect untrained individuals to navigate them. In India, we have Ayurvedic practitioners who understand herb-drug interactions intuitively. Here? We rely on a 7-minute visit and an EHR that flags nothing unless it’s written in neon. The fact that this is still happening in 2025 is not negligence-it is moral failure. Your muscles are not collateral damage. They are your body. Treat them with respect-or pay the price.