When your chest hurts, your brain screams: heart attack. But not every chest pain is a heart attack. And not every heart attack looks like the movies show. Some people feel pressure. Others feel like they’ve been punched in the back. Some don’t feel pain at all-just exhaustion, nausea, or jaw aching. Knowing when to rush to the emergency department could save your life-or someone else’s.
What Counts as Chest Pain?
Chest pain isn’t just a sharp stab or squeezing feeling in your chest. The 2021 American Heart Association guidelines define it broadly: pressure, tightness, burning, or discomfort anywhere in the chest, shoulders, arms, neck, jaw, upper back, or even the upper abdomen. It can come with shortness of breath, cold sweat, nausea, or sudden fatigue. These are called anginal equivalents-signs your heart is struggling, even if you don’t feel classic chest pain.Women, older adults, and people with diabetes are more likely to have these atypical symptoms. A 68-year-old woman might not say, "My chest hurts." She might say, "I just can’t catch my breath," or "I feel like I’ve been run over by a truck." That’s not weakness-it’s a warning.
When to Call 9-1-1 Right Now
Don’t wait. Don’t text a friend. Don’t drive yourself. If you or someone else has chest discomfort plus any of these, call emergency services immediately:- Pressure, tightness, or squeezing in the chest lasting more than 5 minutes
- Pain that spreads to the arm, jaw, neck, or back
- Breaking out in a cold sweat without reason
- Shortness of breath with or without chest pain
- Nausea, vomiting, or sudden dizziness
- Feeling like you’re going to pass out
- Heart rate over 100 beats per minute with no clear cause
- Low blood pressure (below 90 systolic)
These aren’t "maybe" signs. They’re red flags. The average time from symptom onset to hospital arrival for heart attack patients is 2 hours. But the goal is under 60 minutes. Every minute counts. Delaying care increases the chance of permanent heart damage or death.
Why Ambulance Over Your Own Car?
You might think driving yourself is faster. It’s not. Emergency Medical Services (EMS) start treatment before you even get to the hospital. They can grab an ECG in the back of the ambulance, notify the ER team ahead of time, and even begin clot-busting drugs if needed.Studies show people who drive themselves to the ER have a 25-30% higher risk of complications or death compared to those transported by ambulance. Why? Because they’re often alone, in pain, and delayed. Ambulances also have trained staff who can recognize life-threatening rhythms like ventricular fibrillation and deliver a shock if needed-something your car doesn’t have.
What Happens When You Arrive at the ER
Once you’re in the emergency department, time is the priority. The first thing they do? Get an ECG-within 10 minutes of arrival. That’s not a suggestion. It’s a national standard. The ECG can show if you’re having a STEMI (ST-elevation myocardial infarction), the most dangerous type of heart attack. If it does, the team springs into action. The goal? Get you to the cath lab and open the blocked artery within 90 minutes.Next, they’ll check your blood for cardiac troponin-the protein released when heart muscle is damaged. Modern high-sensitivity troponin tests can detect tiny amounts, allowing doctors to rule out a heart attack in as little as 1-2 hours for many patients. This isn’t guesswork. It’s science. In fact, 70-80% of people who come in with chest pain are ruled out for heart attack using this protocol.
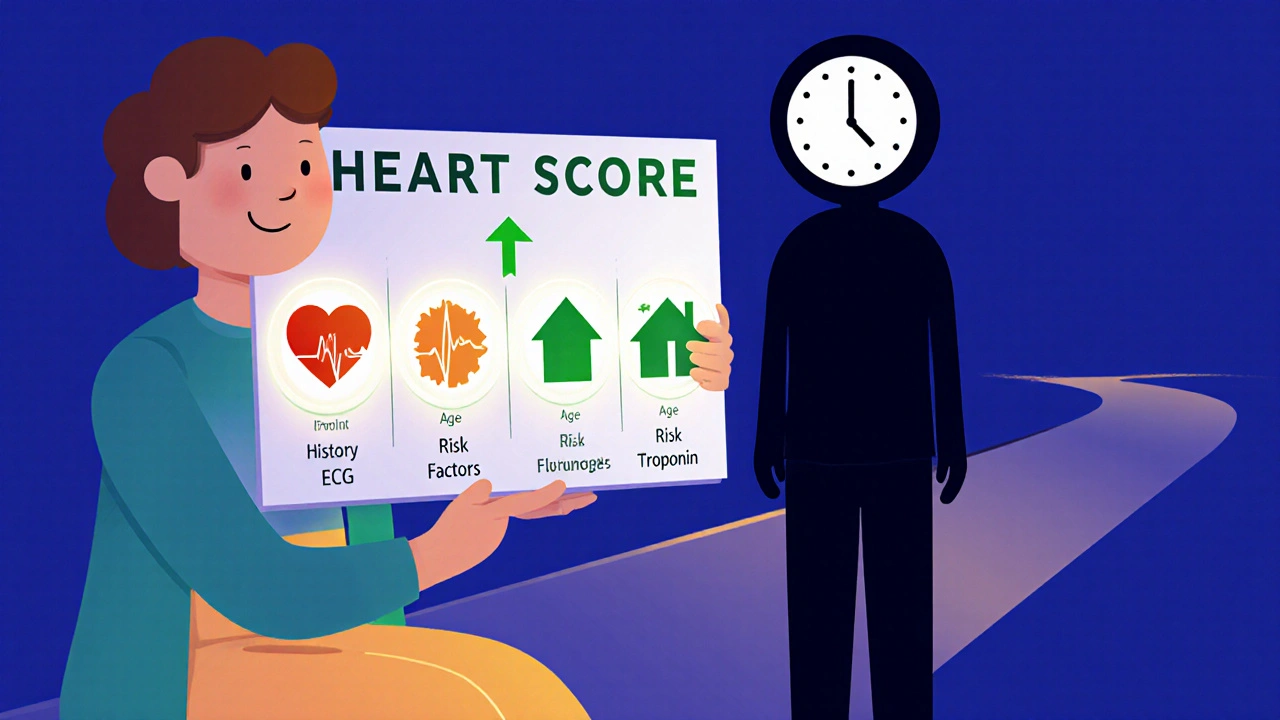
But they won’t stop there. They’ll look at your age, risk factors (like high blood pressure, smoking, diabetes), and symptoms using a tool called the HEART score. A score of 0-3 means low risk. 4-6 means you need more tests. 7-10? That’s high risk-you’re going to the cath lab fast.
What Doesn’t Need the ER
Not every twinge means you need to rush. If you’ve had similar discomfort before, and it goes away with rest or nitroglycerin, and your vital signs are normal, you might be dealing with stable angina. That still needs a doctor’s visit-but not an emergency trip.Other non-cardiac causes of chest pain include:
- Acid reflux (burning after eating, worse when lying down)
- Muscle strain (pain worsens with movement or deep breathing)
- Anxiety or panic attacks (often with tingling hands, rapid breathing, but normal ECG and troponin)
- Lung issues like pneumonia or pleurisy (sharp pain with breathing)
If you’re unsure, it’s always safer to get checked. But if you’re certain it’s your usual heartburn, and you’ve been diagnosed before, you can try an antacid and wait. If it doesn’t improve in 30 minutes, call your doctor. If it gets worse, call 9-1-1.
What You Can Do Before the ER
If you’re experiencing symptoms:- Stop what you’re doing. Sit down. Don’t exert yourself.
- Call 9-1-1 immediately. Don’t wait to see if it gets better.
- If you’re not allergic and have aspirin on hand, chew one 325 mg tablet. It helps thin the blood while you wait.
- Don’t take nitroglycerin unless you’ve been prescribed it and know how to use it.
- Stay calm. Panic makes symptoms feel worse.
Remember: It’s better to be wrong and safe than right and dead.
Why This Matters Now
By 2025, 75% of U.S. hospitals will use AI to help interpret ECGs. These tools can spot subtle changes humans miss-like tiny ST-segment shifts that signal early ischemia. That means faster, more accurate decisions. But AI doesn’t replace you. It helps your doctor act faster.The biggest problem isn’t technology. It’s delay. People wait. They think it’s indigestion. They’re afraid of "bothering" the ER. But emergency departments are built for this. They see 6-8 million chest pain cases every year in the U.S. alone. Only 10-15% turn out to be heart attacks. But if you’re in that 10-15%, every minute you wait reduces your chance of survival.
Final Thought: Don’t Guess. Get Checked.
Chest pain is a signal-not a diagnosis. You can’t tell if it’s your heart by googling symptoms. Only a doctor with an ECG, troponin test, and clinical judgment can say for sure. If you’re uncertain, err on the side of caution. Call 9-1-1. Let the professionals decide.Your heart doesn’t ask for permission before it fails. But you can give it a fighting chance by acting fast.
Can chest pain be caused by something other than a heart attack?
Yes. Many non-cardiac causes exist, including acid reflux, muscle strain, anxiety, lung infections, and costochondritis (inflammation of chest wall cartilage). But because heart-related causes can be deadly, all chest pain must be evaluated by a medical professional before being ruled out as non-cardiac.
Is it safe to wait and see if chest pain goes away?
No. If chest pain lasts more than 5 minutes, especially with other symptoms like sweating, nausea, or shortness of breath, waiting can lead to irreversible heart damage or death. Emergency care should begin immediately-don’t delay.
Do women experience heart attacks differently than men?
Yes. While men often report classic crushing chest pain, women are more likely to have symptoms like fatigue, nausea, jaw or back pain, and shortness of breath without chest discomfort. These atypical signs are often misdiagnosed, leading to delays in treatment.
Can a normal ECG rule out a heart attack?
Not always. Some heart attacks, especially non-ST-elevation types, don’t show clear changes on the first ECG. Doctors rely on serial ECGs and blood tests (troponin) over time to confirm or rule out heart damage. A single normal ECG doesn’t mean you’re safe.
What’s the HEART score and why does it matter?
The HEART score is a clinical tool doctors use to assess risk based on five factors: History, ECG findings, Age, Risk factors (like smoking or diabetes), and Troponin levels. A score of 0-3 means low risk and may allow safe discharge. A score of 7-10 means high risk and requires immediate intervention. It helps avoid both missed heart attacks and unnecessary hospitalizations.
Should I take aspirin if I think I’m having a heart attack?
If you’re not allergic to aspirin and have a 325 mg tablet available, chewing it while waiting for emergency services can help reduce blood clotting. But don’t delay calling 9-1-1 to find aspirin. Emergency response is the priority.
Can stress or anxiety cause chest pain that feels like a heart attack?
Yes. Panic attacks can cause chest tightness, rapid heartbeat, and shortness of breath that mimic heart attack symptoms. But unlike a heart attack, anxiety-related pain usually doesn’t come with elevated troponin levels or ECG changes. Still, it’s impossible to tell the difference without medical testing-so always get checked.
How long does it take to rule out a heart attack in the ER?
With modern high-sensitivity troponin tests and rapid protocols, many patients can be safely ruled out in 1-2 hours. But if symptoms persist or risk factors are high, doctors may extend testing to 3-6 hours to be certain. The goal is accuracy-not speed alone.

Julia Strothers
Let me guess - the ER is just a front for Big Pharma’s profit machine. They *want* you to panic so you’ll get scanned, tested, and hooked on statins for life. I’ve seen the data - 70% of ‘heart attacks’ are just acid reflux mislabeled by overworked interns. And don’t get me started on AI ECGs… they’re trained on corporate datasets that ignore rural populations. You think you’re saving lives? You’re just feeding the machine. Call 9-1-1? Nah. I’ll call my holistic practitioner. She’s got a crystal that vibrates at cardiac frequency.
Erika Sta. Maria
ok so i read this and i was like… wait… what if chest pain is just your soul screaming because capitalism broke you? like seriously. i had this ‘heart attack’ once and it was just my student loan payments haunting me. also why do we even have hospitals? why not just… meditate? or chant? i once cured my migraine by yelling at a cactus. maybe the heart is just tired of being taken for granted. 🤔
Nikhil Purohit
Really appreciate this breakdown - especially the part about atypical symptoms in women and diabetics. I’ve seen my mom dismiss her fatigue as ‘just aging’ until she ended up in the ER with a blocked artery. The HEART score is gold. My uncle got discharged after a normal ECG and came back two days later in arrest - they didn’t do serial troponins. Don’t let a single test fool you. If you’re unsure, go. No shame in being the person who ‘overreacted.’
Debanjan Banerjee
Let’s be brutally honest: the biggest killer here isn’t the heart attack - it’s denial. People delay because they’re afraid of being a burden, or they think ‘it’ll pass.’ It won’t. The data is crystal clear - every minute of delay reduces survival by 10%. Ambulances aren’t just faster - they’re lifesaving ecosystems. ECGs in transit, pre-alerts to cath labs, paramedics trained to recognize VFib - none of that happens if you drive yourself. And aspirin? Yes, chew it. But only after calling 911. Not before. Not instead. This isn’t a suggestion - it’s a protocol written in blood.
Steve Harris
This is one of the most balanced, well-researched pieces I’ve seen on this topic. Thank you. I work in public health, and I’ve seen too many people avoid the ER because they’re worried about cost, or they don’t want to ‘waste’ time. But the truth? The ER sees millions of chest pain cases every year - and 85% of them aren’t heart attacks. That means 15% are. And if you’re in that 15%, you don’t get a second chance. I tell my patients: ‘If you’re asking yourself whether to go, you already know the answer.’
Michael Marrale
So… what if the whole heart attack thing is a scam? I mean, have you ever seen the hospital bills? And why do they always test for troponin but never check for 5G radiation exposure? I read a guy on YouTube who said the ECG machine is actually a mind-control device. And what if the ‘atypical symptoms’ are just your body rejecting corporate medicine? I’ve got a friend who used garlic and lemon juice and his chest pain vanished. Coincidence? I think not. 😏
David vaughan
...I... I had this... uh... weird chest thing last Tuesday... and I... I didn’t go... I... I thought it was just... anxiety... but then I... I read this... and now I’m... shaking... I’m so sorry... I didn’t know... I’m going to the ER tomorrow... I promise... I’ll call 911... I’ll chew the aspirin... I’m sorry... I’m so sorry... I didn’t know... 😭
David Cusack
One must question the epistemological foundations of the HEART score - a crude heuristic derived from population-level aggregates, devoid of ontological nuance. The very notion of 'risk stratification' reduces the human organism to a statistical artifact. And AI? A digital idolatry. One wonders whether the algorithm has ever felt the weight of existential dread manifesting as cardiac discomfort. The ER is not salvation - it is the temple of institutionalized fear. One should perhaps simply sit quietly... and listen to the silence within.
Elaina Cronin
As a nurse of 22 years, I have witnessed too many patients arrive too late because they were told, 'It's probably just indigestion.' I have held the hands of women who didn't scream for chest pain - they whispered, 'I'm just so tired.' And then they died. This post is not just informative - it is a moral imperative. If you are reading this and you’ve ever dismissed your symptoms because you didn't 'look sick' - please, for the love of all that is holy, change. Call 911. Not tomorrow. Not after dinner. Now.
Willie Doherty
While the clinical guidelines presented are statistically sound, the underlying assumption that emergency intervention is always optimal warrants scrutiny. The data on ambulance transport superiority is confounded by selection bias - those who call 911 are often sicker at baseline. Moreover, the overutilization of troponin assays has led to diagnostic creep, with false positives triggering cascades of unnecessary catheterizations. The true epidemic is not delayed care - it is medical overreach disguised as vigilance. One must ask: are we saving lives - or simply prolonging the healthcare industrial complex?