Every year, Americans spend over $650 billion on prescription drugs. That’s more than any other country in the world. And yet, 9 out of 10 prescriptions filled are for generic drugs. The math doesn’t add up-unless you understand how generics are the quiet backbone of affordable healthcare.
Generics Are 80-85% Cheaper, But Still Just as Effective
When a brand-name drug loses its patent, generic versions hit the market. They’re not cheaper because they’re lower quality. They’re cheaper because they don’t need to repeat the $2.6 billion in research and clinical trials that went into the original drug. The FDA requires generics to have the exact same active ingredient, strength, dosage form, and route of administration as the brand-name version. And they must prove they work the same way in the body through bioequivalence testing.
That testing isn’t simple. Manufacturers must show that the generic drug is absorbed into the bloodstream at the same rate and to the same extent as the brand-name drug-within a narrow 80% to 125% range. That’s not a guess. It’s a legal requirement backed by blood tests on 24 to 36 healthy volunteers, taken at 12 or more time points over 72 hours. The FDA doesn’t approve a generic unless the data proves it’s therapeutically equivalent.
Real-world results? A 2024 study of 1.2 million patient reviews on Drugs.com showed generics had nearly identical efficacy ratings (4.2/5) compared to brand-name drugs (4.3/5). But when it came to affordability, generics scored 4.5/5. Brand-name drugs? Just 2.3/5. People aren’t just saving money-they’re sticking to their treatment plans.
Generics Saved $445 Billion in 2023 Alone
Here’s the number that tells the whole story: in 2024, generics made up 90% of all prescriptions filled in the U.S.-but only 12% of total drug spending. Brand-name drugs? Just 10% of prescriptions, but 88% of the cost.
That means for every $100 spent on prescriptions, $88 went to brand-name drugs, and only $12 went to generics. But those $12 bought 9 out of every 10 pills. The math is brutal: if generics didn’t exist, the U.S. would be spending over $700 billion more per year on drugs.
That’s not hypothetical. In 2023, generics saved the system $445 billion. That’s more than the entire annual budget of the Department of Education. And it’s growing. The Association for Accessible Medicines estimates that generics saved patients $98 billion in 2024 alone, while brand-name drugs cost $700 billion.
Why Do Brand-Name Drugs Cost So Much?
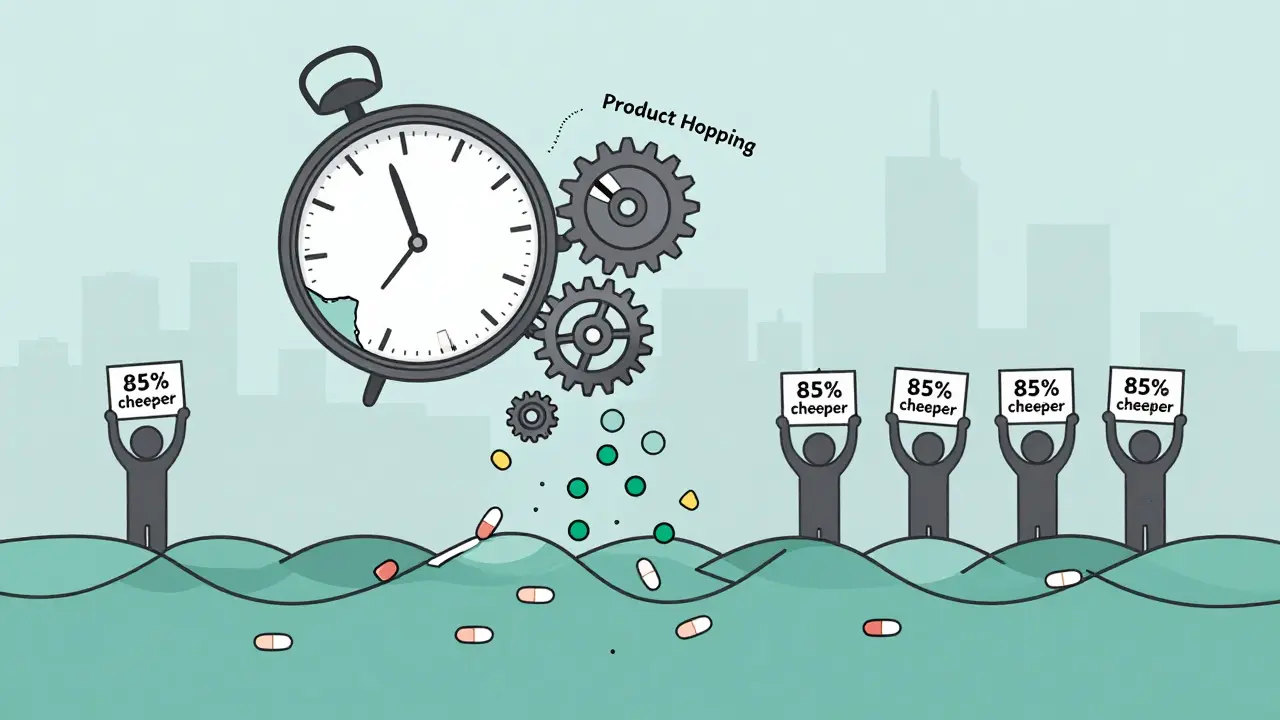
It’s not just about R&D. The real cost drivers are hidden in the system. Patent extensions, pay-for-delay deals, and product hopping are tactics brand manufacturers use to delay generic entry.
Take pay-for-delay: a brand company pays a generic maker to stay off the market. The Federal Trade Commission found these deals delay generic entry by an average of 17 months. That costs consumers $3.5 billion a year in higher prices. In one case, a drug that should have gone generic in 2018 didn’t get a competitor until 2022-all because of a secret payment deal.
Product hopping is another trick. A company slightly changes the pill-say, from a tablet to a capsule-and files a new patent. That resets the clock. Even though the new version isn’t better, pharmacies can’t substitute the generic without a new prescription. The FTC found some drugs have over 140 patents piled on top of each other to block competition.
And then there’s the rise of authorized generics-where the brand company launches its own generic version. It sounds like competition, but it’s not. The price drops, but only by 25-30%, not the 80-85% you’d see from a true independent generic manufacturer. The brand keeps the profit, and patients pay more than they should.
Biosimilars Are the Next Frontier-But They’re Lagging
Biologic drugs-like insulin, rheumatoid arthritis treatments, and cancer therapies-are complex molecules made from living cells. They can’t be copied exactly, so their cheaper versions are called biosimilars.
Biosimilars aren’t as cheap as small-molecule generics. They’re 15-35% cheaper than the brand, not 80%. But they’re still a huge win. Humira, for example, cost $70,000 a year before biosimilars. Now, with biosimilar options, it’s under $50,000.
But here’s the problem: 90% of biologics that are about to lose patent protection in the next five years have no biosimilar in development. In Europe, 70-85% of biologic prescriptions are filled with biosimilars. In the U.S.? Just 25-30%. Why? Because pharmacy benefit managers (PBMs) still favor the brand-name drug through rebates. Even if a biosimilar is cheaper, the PBM gets a bigger kickback from the brand. So they push the more expensive option.
That’s changing slowly. The FDA has a Biosimilars Action Plan to speed up approvals. But without policy changes to stop rebate-driven formularies, biosimilars won’t reach their potential. The Congressional Budget Office estimates biosimilars could save $133 billion by 2025-if they’re allowed to compete fairly.
Generics Aren’t Perfect-But They’re the Best Tool We Have
There are real concerns. Some patients report side effects after switching to a generic-mostly from inactive ingredients like fillers or dyes. In 2023, the FDA logged 1,247 adverse event reports tied to generic substitutions. Most were mild: stomach upset, rashes. But for drugs with a narrow therapeutic index-like warfarin, levothyroxine, or lithium-even tiny differences in absorption can matter.
One patient on PatientsLikeMe shared that after switching from brand-name Synthroid to a generic levothyroxine, she developed fatigue, weight gain, and brain fog. Her doctor switched her back. Her labs were technically “in range,” but she didn’t feel right. That’s not a failure of the generic. It’s a failure of the system to account for individual variation.
That’s why 12 states still require doctors to explicitly authorize substitution for these drugs. Pharmacists can’t just swap them out. It’s a safety net.
But here’s the flip side: when generics aren’t available, patients skip doses. GoodRx’s 2024 report found 68% of people skipped pills or split them to stretch their supply. Among Medicare Part D users, 42% skipped doses because of cost-compared to just 12% when generics were available.
Generics don’t just save money. They save lives.
Why Medicare’s New Drug Negotiation Isn’t Enough
The Inflation Reduction Act let Medicare negotiate prices for 10 drugs in 2026. The savings? 38-79% per drug. That’s huge. But those 10 drugs are just a drop in the bucket.
Medicare covers 32% of U.S. drug spending. The other 68%? Commercial insurers, Medicaid, and out-of-pocket payments. And those systems don’t get the same negotiation power.
The Congressional Budget Office says Medicare negotiation could save $500-550 billion over 10 years. But they also say: “Generic substitution produces substantially greater savings per drug than negotiation.” Why? Because negotiation only works on a few drugs. Generics work on thousands.
Take insulin. Before the Inflation Reduction Act, one vial cost $350. Now, Medicare beneficiaries pay $35. But the same price drop happened across commercial markets-because generic insulin lispro was already available for $25. The cap didn’t create the savings. The generic did.
Who’s Making Generics-and Where?
The U.S. doesn’t make most of its generic drugs. About 80% of the active ingredients come from India and China. That became a problem during the pandemic. When factories shut down, 300+ drug shortages hit the U.S. Most were generics-because no one else was making them.
Today, the biggest generic manufacturers are Teva (10.2% market share), Viatris (8.7%), and Sandoz (7.9%). But companies like Sun Pharma and Dr. Reddy’s control 40% of the API supply chain. That’s a risk. If geopolitical tensions or regulatory crackdowns hit those countries, U.S. patients feel it first.
That’s why some experts are pushing for domestic manufacturing incentives. But for now, the system works-because the cost savings are too big to ignore.
What You Can Do
If you’re on a prescription, ask your doctor or pharmacist: “Is there a generic?” If there is, it’s almost always the better choice. If your insurance charges you more for the generic than the brand, ask why. That’s backward. It’s usually because the pharmacy benefit manager is getting a rebate from the brand company.
Use tools like GoodRx or the FDA’s Orange Book to check if your drug has a generic, and what the price difference is. If you’ve had a bad reaction after switching, tell your doctor. It’s not common, but it happens. And if your drug has a narrow therapeutic index, make sure your prescription says “Dispense as Written” if you need the brand.
Generics aren’t magic. But they’re the most powerful tool we have to control drug spending. They’re safe. They’re effective. And they’re saving billions every year.
Are generic drugs as safe as brand-name drugs?
Yes. The FDA requires generics to meet the same strict standards for safety, strength, purity, and quality as brand-name drugs. They must prove bioequivalence-meaning they work the same way in the body. Over 90% of prescriptions in the U.S. are generics, and they’ve been used safely for decades.
Why do some people say generics don’t work as well?
In rare cases, patients report differences after switching-usually with drugs that have a narrow therapeutic index, like levothyroxine or warfarin. These drugs require very precise dosing. Even tiny variations in absorption can affect how you feel. While generics are still considered therapeutically equivalent, some patients respond better to one formulation over another. If you notice symptoms after switching, talk to your doctor. You may need to stick with the brand.
Can pharmacists substitute generics without my doctor’s permission?
In 48 states, pharmacists can substitute a generic for a brand-name drug unless the prescription says “Dispense as Written.” But 12 states require doctor approval for certain high-risk drugs like seizure medications or thyroid hormones. Always check your state’s rules, and ask your pharmacist if substitution is happening.
Why is my generic more expensive than the brand?
That shouldn’t happen-and usually doesn’t. If your copay for the generic is higher, it’s likely because your insurance plan’s pharmacy benefit manager (PBM) is getting a bigger rebate from the brand-name drug manufacturer. This is called a “generic differential.” Ask your insurer to explain your copay structure. You can often switch to a plan that doesn’t penalize generics.
Will Medicare’s new drug price negotiation make generics obsolete?
No. Medicare’s negotiation applies to only 10 drugs in 2026-and only for Medicare beneficiaries. Generics affect thousands of drugs across all payers. Even the Congressional Budget Office says generic competition delivers more savings per drug than negotiation. Negotiation helps a few expensive drugs. Generics help everyone.

Lily Lilyy
Generics are a miracle for regular folks who just need to take their meds without going broke. I’ve been on levothyroxine for years, and the generic saved me over $200 a month. No side effects, no drama. Just health.
People who say generics don’t work are usually the ones who never had to choose between medicine and groceries. Thank you for this post.
Gabrielle Panchev
Let’s be perfectly, absolutely, undeniably clear-there is a systemic, corporate, profit-driven conspiracy here, and it’s not just about patents or pay-for-delay-it’s about the entire pharmaceutical-industrial complex being designed to extract every possible dollar from sick people, while pretending to care, and yes, I’ve read the FTC reports, the Congressional Budget Office analyses, the FDA’s own internal memos, and the whistleblower testimonies from Indian API plants-and the truth is, we’re being lied to on a structural level, and no, generics aren’t the full solution because they’re still manufactured in countries where labor rights are nonexistent and regulatory oversight is a joke, and yes, I know that sounds paranoid, but when your insulin costs $350 and the generic is $25, and the company that made the original still owns 70% of the market through subsidiaries, then maybe paranoia is the only rational response-
Katelyn Slack
i just wanted to say thank you for writing this. i switched to generic metformin last year and my blood sugar is better than ever. i had no idea generics were this rigorously tested. i thought they were just cheap knockoffs. my pharmacist even explained the bioequivalence thing to me and i was shocked. also, i think i spelled bioequivalence wrong. oops.
Melanie Clark
They’re letting China and India control our medicine supply and you’re celebrating generics? Wake up. The FDA approves these drugs based on paperwork from factories that have never been inspected. The 2020 shortages? That was a warning. The real cost isn’t just money-it’s lives. And now they want to replace brand drugs with generics made in a country that’s actively hostile to us? This isn’t healthcare-it’s surrender.
And don’t even get me started on the PBM rebates. It’s all rigged. The system is designed to make you dependent. They want you weak. They want you buying meds from overseas while their lobbyists write the laws. You think this is about savings? No. It’s about control.
Harshit Kansal
Bro, I’ve been on generic lisinopril for 5 years. Zero issues. My mom switched from brand-name insulin to generic and now she can afford to see her doctor every month instead of skipping visits. India and China make these drugs because they’re good at it. Let’s not pretend we’re the only ones who can do anything right.
Also, why is my copay for the generic higher? That’s messed up. My pharmacist said it’s because the PBM gets paid more from the brand. I’m switching plans next month.
Brian Anaz
Let’s cut the nonsense. We don’t need to be grateful for generics-we need to demand American-made medicine. Why are we outsourcing the most critical part of our healthcare to foreign regimes? The FDA says they’re equivalent? Fine. But what about national security? What happens when the supply chain breaks again? We’re not saving money-we’re surrendering sovereignty.
And don’t act like generics are perfect. They’re a Band-Aid on a bullet wound. The real solution? Bring manufacturing home. Stop letting foreign governments dictate our health.
Venkataramanan Viswanathan
As someone who works in pharmaceutical logistics in India, I can confirm: the quality control standards for generics exported to the U.S. are among the strictest in the world. Our factories undergo FDA inspections more frequently than many U.S. plants.
The real issue isn’t where the drugs are made-it’s how the U.S. system rewards monopolies instead of competition. Generics are not the problem. The rebate system, patent abuse, and lack of price transparency are.
And yes-we are proud to make these medicines. They save lives, not just dollars.
Vinayak Naik
Generics are the unsung heroes of American healthcare-like the quiet kid in class who aced the test but never bragged about it.
My cousin was on Humira for RA-$70K a year. Switched to a biosimilar? $45K. Same results. She’s hiking again. No magic, no hype-just smart science and a system that finally let competition do its job.
And yeah, some folks feel weird switching, especially with thyroid meds. That’s real. But that’s not the generic’s fault-it’s the system’s failure to personalize care. Doctors need to listen more, not just check labs.
Also, GoodRx is your BFF. Use it. It’s like a coupon for your soul.
Saylor Frye
It’s fascinating how the article romanticizes generics as if they’re some grassroots triumph of the people, when in reality, they’re a byproduct of corporate arbitrage and regulatory capture. The FDA’s bioequivalence standards are laughably lenient-80% to 125%? That’s a 45% variance. It’s not science; it’s a compromise.
And let’s not pretend the savings are distributed evenly. The real beneficiaries are insurers and PBMs, not patients. The $445 billion saved? That’s not money in your pocket-it’s profit shifting.
Generics aren’t the answer. They’re the illusion of one.
Kiran Plaha
I’ve been wondering-why don’t more people know about the Orange Book? I found out about it last year when I was comparing prices for my blood pressure med. Turns out, there are 5 different generics, and one costs $4. The others are $20+. Why isn’t this common knowledge?
Also, I asked my pharmacist why my copay was higher for the generic, and she said it’s because my plan’s PBM gets a rebate from the brand. I didn’t even know PBMs existed until then.
Maybe we need a public education campaign. Not just for generics, but for how the whole system works. People shouldn’t need to be detectives just to afford their medicine.