When you start treatment for osteoporosis, waiting a full year or two to see if it’s working can feel like gambling with your bones. That’s where bone turnover markers come in-they give you a real-time snapshot of what’s happening inside your skeleton, long before a DEXA scan can show any change.
What Are Bone Turnover Markers?
Bone isn’t static. Every day, old bone breaks down and new bone forms. This process, called remodeling, is normal. But in osteoporosis, the balance tips: bone breaks down faster than it rebuilds. Bone turnover markers (BTMs) are tiny proteins and fragments released into your blood or urine when bone is being broken down or built up. They’re like smoke signals from your bones-telling you whether the treatment is quieting the breakdown or sparking new growth.
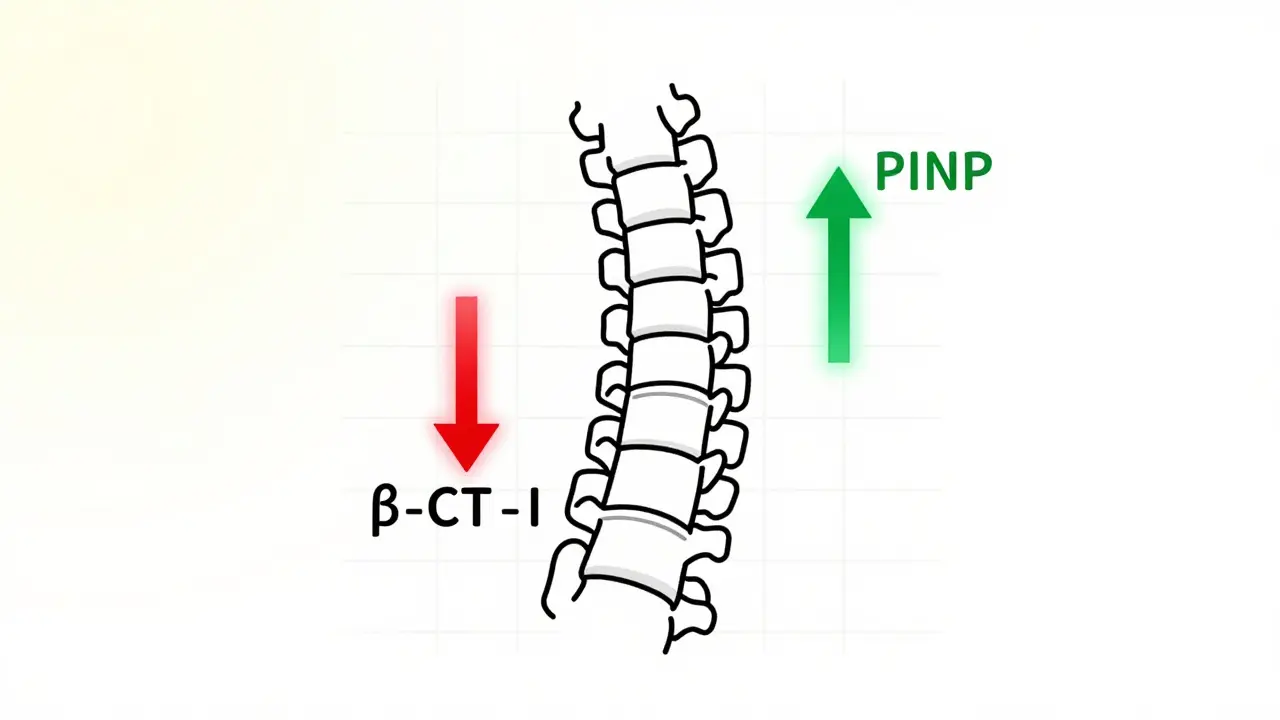
There are two main types: resorption markers and formation markers. Resorption markers, like β-CTX-I, show how fast bone is being broken down. Formation markers, like PINP, show how fast new bone is being made. The two most reliable ones used today are serum PINP and plasma β-CTX-I. These aren’t just research tools-they’re now the gold-standard clinical markers recommended by the International Osteoporosis Foundation and the European Calcified Tissue Society in their 2023 consensus guidelines.
Why They Matter More Than You Think
Think of your bone density scan (DEXA) as a photo of your skeleton. It shows you how much bone you have left, but it’s slow to change. It takes 12 to 24 months to see a clear improvement after starting medication. By then, if the drug isn’t working, you’ve already been taking it for a long time-possibly with side effects, and possibly still at risk for fractures.
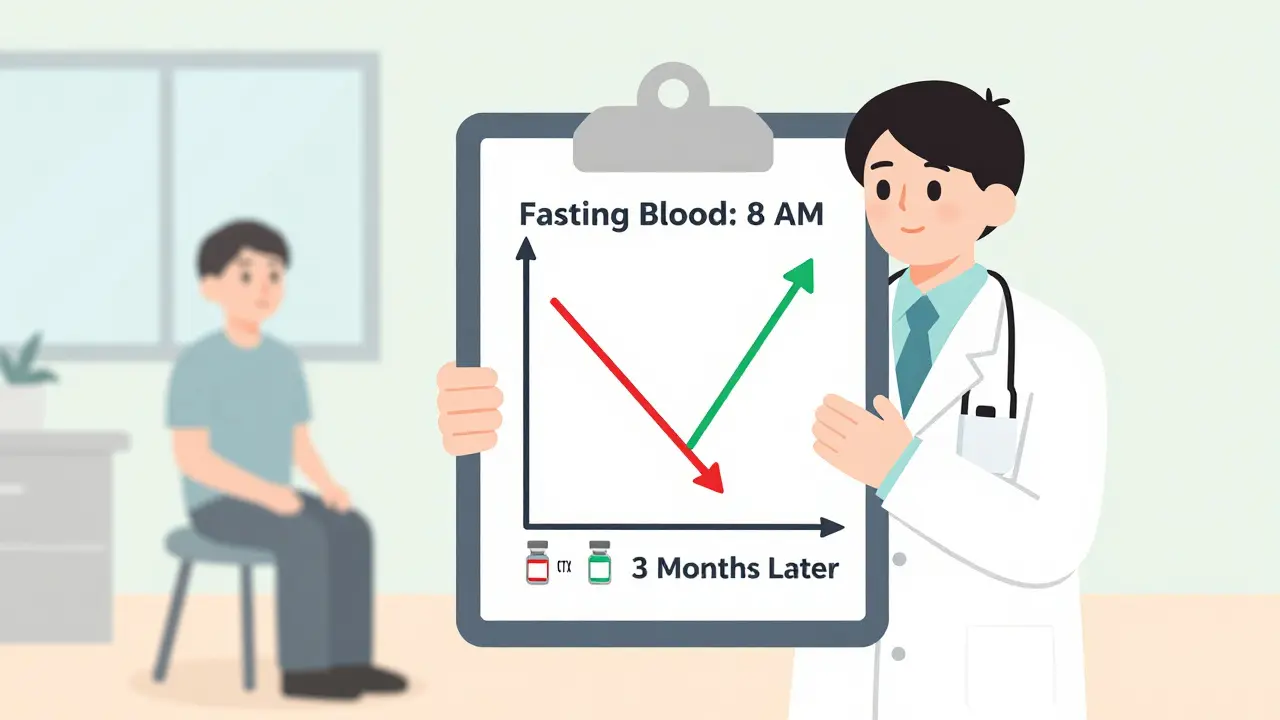
Bone turnover markers change much faster. Within 3 to 6 weeks of starting a drug like alendronate or denosumab, you’ll see a drop in β-CTX-I. A 30% or greater decrease in this marker by 3 months is a strong sign the treatment is working. For anabolic drugs like teriparatide, PINP spikes-often doubling or tripling in just a few months. That’s your body’s way of saying, “New bone is being built.”
This early feedback is powerful. It tells you whether you’re responding to treatment before it’s too late. If your markers don’t move, it could mean you’re not taking the medication, your body isn’t absorbing it, or the drug just isn’t right for you. That’s not something a DEXA scan can tell you until it’s too late.
How Doctors Use Them in Practice
Here’s how it actually works in a clinic:
- Before treatment: A baseline blood test is done for PINP and β-CTX-I. This gives you a starting point.
- At 3 months: You get tested again. If β-CTX-I dropped more than 25% (or PINP rose more than 35% for anabolic drugs), you’re on track. If not, your doctor might check your adherence, adjust the dose, or switch therapies.
- At 12-24 months: You get your DEXA scan. This confirms whether the bone density improved. But by now, you already knew if the treatment was working-thanks to the BTMs.
This approach isn’t theoretical. The TRIO study showed patients who hit a 30% drop in β-CTX-I at 3 months had a 1.6% lower fracture risk after just 22 weeks compared to those who didn’t. That’s a measurable difference in real-world outcomes.
What You Need to Know Before Getting Tested
Bone turnover markers are sensitive. A small mistake in how the test is done can throw off the results.
- Fast before β-CTX-I tests. Eat or drink anything after midnight, and your CTX levels can jump 20-30%. Fasting is mandatory.
- Test in the morning. CTX levels rise and fall with your circadian rhythm. The best time to draw blood is between 8 and 10 a.m. PINP is less affected, but morning is still preferred for consistency.
- Same lab, same method. Different labs use different machines and reagents. If you switch labs, your results might look different-even if your bone health hasn’t changed. Stick with one lab for all your tests.
- Don’t test right after a fracture or surgery. Bone healing spikes turnover markers. Wait at least 6-8 weeks after any major bone trauma.
These aren’t just minor details-they’re critical. A 2022 review in Endocrine Reviews found that preanalytical errors (like not fasting or testing at the wrong time) are the #1 reason BTMs get misinterpreted.
Who Should Get Them-and Who Doesn’t Need Them
BTMs aren’t for everyone. They’re most useful when:
- You’ve just started osteoporosis treatment and want early confirmation it’s working.
- You’re on an anabolic drug like teriparatide or romosozumab, where fast feedback is key.
- You’re not responding to treatment as expected, and your doctor suspects poor adherence or drug resistance.
- You have chronic kidney disease (CKD). In CKD, traditional markers like PINP and CTX can be falsely elevated due to reduced clearance. In these cases, bone alkaline phosphatase (BALP) or TRACP5b are better alternatives.
But if you’re just getting diagnosed and haven’t started treatment yet, a DEXA scan is enough. If you’ve been on the same medication for 3+ years and feel fine, BTMs add little value. They’re not meant to replace DEXA-they’re meant to work alongside it.
Limitations and What’s Still Unknown
Bone turnover markers aren’t perfect. They reflect whole-body bone activity, not what’s happening in your hip or spine. A drop in β-CTX-I doesn’t tell you whether your spine is strengthening-just that bone breakdown has slowed overall.
There’s also biological variability. Even in healthy people, BTM levels can swing 20-60% day to day. That’s why the “least significant change” matters: a 25% drop in CTX or 20% rise in PINP is the minimum to count as real. Smaller changes? Probably just noise.
Another issue: reference ranges. Most normal values are based on Caucasian populations. Studies show Asian individuals often have 15-20% lower baseline CTX levels, and African populations tend to have higher PINP. Without population-specific ranges, you risk overtreating or undertreating people from different ethnic backgrounds.
And while Medicare and many European insurers cover these tests, not all do. In the U.S., only about 25-35% of clinics routinely use them, partly because many doctors aren’t trained to interpret them.
The Future: Smarter, Faster, More Personal
The field is moving fast. Clinical trials like NCT04567821 are testing whether using BTMs to guide treatment decisions leads to fewer fractures than standard care. Point-of-care tests-where a nurse can get results in minutes instead of days-are in development. If approved, these could make BTMs as routine as checking your blood pressure.
Researchers are also looking at combining BTMs with AI to predict fracture risk more accurately. Imagine a model that takes your PINP level, age, BMI, and past fractures-and tells you your 1-year fracture risk with 90% accuracy. That’s not science fiction anymore.
For now, the message is clear: bone turnover markers are no longer experimental. They’re a proven, practical tool for monitoring osteoporosis therapy. They give you control, clarity, and confidence-before your bones have a chance to break.
What to Ask Your Doctor
If you’re on osteoporosis treatment, here are three questions to ask at your next visit:
- “Have I had a baseline bone turnover marker test? If not, can we do one before I start or change meds?”
- “When should I get retested? And what results would tell us the treatment is working?”
- “Is my lab using the standardized methods for PINP and β-CTX-I? Can you confirm they follow IFCC guidelines?”
These aren’t just smart questions-they’re essential ones. Your bones are counting on it.
Are bone turnover markers better than DEXA scans for monitoring osteoporosis?
No-they’re not better, they’re complementary. DEXA scans measure bone density and are the gold standard for diagnosis and long-term monitoring. But they take 1-2 years to show change. Bone turnover markers show treatment response in 3-6 months. Use both: BTMs for early feedback, DEXA for final confirmation.
Can I do a bone turnover marker test at home?
Not yet. All current BTM tests require a blood draw and lab analysis. Some companies are developing point-of-care devices, but none are approved for routine clinical use as of early 2026. Don’t trust home kits or unverified tests-they’re not validated.
Why does fasting matter for β-CTX-I?
Food intake, especially protein, triggers a temporary spike in bone breakdown. Eating before the test can raise β-CTX-I levels by 20-30%, making it look like your bone loss is worse than it is. Fasting ensures the result reflects your true bone metabolism, not your breakfast.
What if my bone turnover markers don’t change after 3 months?
It doesn’t automatically mean the drug failed. First, check if you took the medication as prescribed. Missed doses are the #1 reason for no response. If adherence is good, your doctor may repeat the test, check for kidney issues, or consider switching to a different class of drug-like switching from a bisphosphonate to an anabolic agent.
Are bone turnover markers covered by insurance?
In the U.S., Medicare covers PINP (CPT 83970) and β-CTX-I (CPT 83935) for osteoporosis monitoring since 2020. Many private insurers follow suit, but coverage varies. Always check with your provider before testing. In Europe and Australia, coverage is more consistent due to official guidelines.
Siobhan Goggin
This is exactly the kind of practical, science-backed advice I wish more doctors gave. I started denosumab last year and felt lost until my endocrinologist ordered the PINP and β-CTX-I tests. Seeing that 40% drop in CTX at 3 months gave me peace of mind I didn’t know I needed.
Vikram Sujay
One must consider the epistemological foundations of biomarker interpretation in clinical practice. The reductionist reliance on serum PINP and β-CTX-I, while statistically significant, may obscure the phenomenological reality of individual bone metabolism. The body is not a machine to be calibrated, but a dynamic system whose signals must be interpreted with humility and contextual awareness.
Jay Tejada
So let me get this straight - we’re paying hundreds of dollars to check if our bones are getting the memo that they’re supposed to stop falling apart? And the only thing we’re told to do is... not eat breakfast? I’m just saying, if my bones need a 6 a.m. lecture on fasting, maybe we’re doing this wrong.
Shanna Sung
They're lying to you about the markers. The pharmaceutical companies pushed this because DEXA scans were too slow to keep you hooked on drugs. They want you to think you're failing if your CTX doesn't drop. But what if your bones are just naturally quiet? What if they're testing you because they want to sell you more pills? I read a whistleblower report once...
mark etang
As a clinical researcher with over two decades in metabolic bone disease, I can confirm that the International Osteoporosis Foundation's 2023 guidelines represent a paradigm shift. The integration of PINP and β-CTX-I into routine monitoring protocols is not merely evidence-based - it is ethically imperative. Failure to implement these standards constitutes a breach of the standard of care.
Brendan F. Cochran
Y’all are overcomplicating this. I’m a mechanic. I fix cars. I don’t need some fancy lab test to tell me if my car’s engine is running. I just check the oil. Same thing with bones. If you’re not taking your pills, your bones are gonna break. Stop overthinking it. Just take the damn medicine and eat your damn calcium.
Charlotte N
Wait so if I get my test done at 11am instead of 9am, does that mean my results are useless? And what if I had coffee without sugar? Does that count as breaking the fast? And what if my lab switched machines last year but I didn’t know? Am I just supposed to guess? This feels like a minefield. I just want to know if I’m gonna break a hip.
bob bob
I’ve been on alendronate for 4 years and never had a BTM test. My DEXA was stable. I feel fine. But now I’m wondering - did I miss something? Should I go back and get tested? I don’t want to be one of those people who finds out too late. Maybe I’ll ask my doc next time.
Uzoamaka Nwankpa
Everyone keeps talking about the science like it’s magic, but no one talks about how hard it is to get these tests covered. I had to fight my insurance for 3 months just to get PINP approved. I’m on disability. I can’t afford to pay $300 out of pocket every 3 months just to prove I’m not failing. Who benefits from this? Not me.
Chris Cantey
The real question isn’t whether BTMs work - it’s whether we’ve been conditioned to believe that our bodies need constant surveillance. We’ve been taught that biology is a dashboard to be monitored, that health is a metric to be optimized. But what if the act of measuring itself is the disease? What if our bones are whispering, and we’ve learned to scream for answers?
Abhishek Mondal
Let me clarify, for those who may be unaware: the IFCC guidelines, while authoritative, are fundamentally Eurocentric in their derivation. The referenced 2022 Endocrine Reviews paper, while competent, fails to adequately address the confounding influence of vitamin D receptor polymorphisms in South Asian populations - a critical oversight, particularly given the global burden of osteoporosis in India and Southeast Asia. One must question the universality of a 30% threshold when baseline CTX in Indian women averages 18% lower than in Caucasians.
Oluwapelumi Yakubu
Man, I love this. Real talk - this is the kind of info that should be plastered on billboards, not buried in medical journals. My aunt broke her hip last year, and nobody ever told her about these markers. She was on meds for a year and thought she was fine - until she wasn’t. If we can catch this early, we can save people from the hospital, the rehab, the loneliness after. This ain’t just science - it’s justice.