When your monthly medication bill feels like a punch to the gut, you’re not alone. Nearly 3 in 10 Americans skip doses, split pills, or skip refills because they can’t afford their prescriptions. The good news? There’s a proven way to cut those costs without sacrificing your health: asking for a therapeutic alternative.
This isn’t about generics. It’s not about coupons or discount cards. It’s about swapping one effective medication for another that works just as well-but costs a fraction of the price. And yes, you can ask for it. Here’s how.
What Is a Therapeutic Alternative?
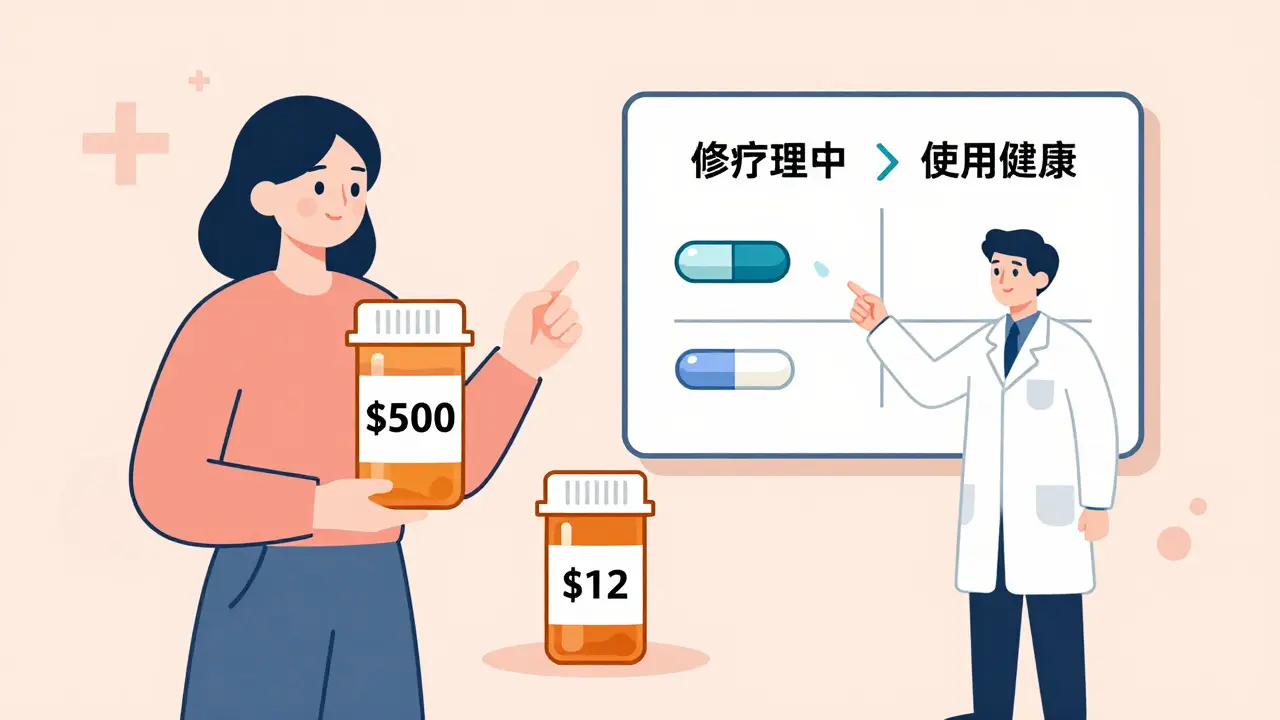
A therapeutic alternative is a different drug that treats the same condition as your current medication, but isn’t chemically identical. For example, if you’re taking brand-name Eliquis (apixaban) for blood clots, your doctor might suggest switching to generic warfarin. Both prevent clots. Both are FDA-approved. But warfarin costs about $10 a month instead of $500.
Unlike generic substitution (where you get the exact same drug in a cheaper form), therapeutic interchange lets you switch to a different chemical entirely. Think of it like choosing between two different brands of pain reliever: ibuprofen and naproxen. Both work. One might be cheaper. Your doctor just needs to know which one fits your body and your budget.
According to a 2023 study from the American Academy of Family Physicians, 23% of adults don’t fill prescriptions because of cost. Therapeutic alternatives can fix that. A Vanderbilt University study found that when doctors proactively offered these switches, patients saved an average of $17.77 per month-without any drop in health outcomes.
When Does It Work?
Not every drug has a cheaper cousin. But for many common conditions, the options are plentiful.
- Blood pressure: Lisinopril (generic) instead of Benicar or Cozaar. Savings: $300+/month.
- Cholesterol: Atorvastatin (generic) instead of Crestor. Savings: $380/month.
- Acid reflux: Omeprazole (generic) instead of Nexium. Savings: 96%-from $365 to $15 a month.
- Diabetes: Metformin instead of Jardiance or Ozempic. Savings: $400+/month.
- Depression: Sertraline instead of Lexapro or Zoloft. Savings: $100+/month.
These aren’t hypotheticals. These are real switches made every day in clinics across the country. The key? You need to know what’s available.
Use tools like GoodRx or your local pharmacy’s $4 generic list. Enter your current drug. See what else works. Then bring that list to your doctor. Don’t ask, “Is there a cheaper option?” Ask, “Can I switch to omeprazole instead of esomeprazole?” Specificity gets results.
How to Ask Your Doctor
Doctors aren’t against saving you money. Many don’t even know what’s affordable. A 2023 survey found that 37% of patients had trouble convincing their provider to consider a switch.
Here’s how to make it easier:
- Start with your budget. Say: “I’m struggling to afford my current meds. I’ve been looking at alternatives and found a few that might work.”
- Bring proof. Print out a GoodRx price comparison. Show them the cost difference. Example: “Eliquis is $480/month. Warfarin is $12. Both are approved for atrial fibrillation.”
- Use the right language. Don’t say, “Can I get a cheaper pill?” Say, “Is there a therapeutically equivalent option that’s more affordable?” That’s the term doctors recognize.
- Be ready to try. Sometimes, you’ll need to switch and give it 2-4 weeks. Your body might respond differently. That’s okay. Track how you feel. Report back.
Doctors are more open than you think. A 2024 study showed that when patients came in with specific alternatives already researched, doctors agreed to the switch 82% of the time.

What If Your Doctor Says No?
They might say: “That’s not as effective.” Or “It’s not right for your condition.” Sometimes, they’re wrong. Sometimes, they’re cautious.
Here’s what to do next:
- Ask why. “What’s the clinical reason you’re hesitant?” If they say, “I’ve never tried it,” that’s not a medical reason. If they say, “It’s not as effective in patients with kidney disease,” then you’ve got a real concern.
- Request a trial. “Can we try it for 30 days? If it doesn’t work, we go back.” Many doctors will agree if you’re willing to monitor.
- Ask for a tiering exception. If you’re on Medicare Part D, your plan might cover your current drug at a higher cost. You can request an exception. Fill out a form. Your doctor signs it. CMS requires a decision within 72 hours for urgent cases.
- Get a second opinion. Go to a different primary care provider or a pharmacist. Many pharmacies now have clinical pharmacists who specialize in cost-saving switches.
One patient, a 68-year-old woman on Lyrica for nerve pain, was told by her neurologist that gabapentin wouldn’t work. She got a second opinion. The new doctor said, “It’s the same mechanism. Let’s try it.” She saved $435/month. And her pain stayed under control.
Other Ways to Cut Costs (While You Wait)
Therapeutic alternatives are powerful-but they take time. In the meantime, use these tools:
- 90-day supplies: Ask for a 3-month prescription. It cuts copays by 25% and reduces trips to the pharmacy.
- Manufacturer coupons: Many brand-name drugs have free or low-cost coupons (like $0 co-pays). Check the drug’s official website.
- Patient assistance programs: Organizations like NeedyMeds, RxAssist, and the HealthWell Foundation help low-income patients get meds for free. Income must be under $60,000/year for individuals.
- Compare pharmacy prices: A 2023 GoodRx report found prices can vary by 5,000% between pharmacies. A drug that costs $200 at CVS might be $15 at Walmart.
Pro tip: Use GoodRx’s app. It shows real-time prices at pharmacies near you. Print or screenshot the lowest price. Take it to the pharmacy. They’re legally required to honor it-even if you’re insured.

When It Won’t Work
Therapeutic interchange isn’t magic. It doesn’t work for everything.
- Biologics: Drugs like Humira, Enbrel, or Orencia have no generic or therapeutic alternatives. These are complex proteins made from living cells. No simple swap exists.
- Specialty drugs: Cancer, rare disease, and transplant medications often have no cheaper alternatives. That’s why 30% of drug costs come from these.
- Patients with complex conditions: Someone with multiple chronic diseases might respond poorly to a switch. Your doctor needs to weigh risks carefully.
But here’s the thing: only 15% of medications fall into this category. For the other 85%, there’s almost always a better option.
Why This Matters Long-Term
Let’s say you take a blood pressure pill that costs $120/month. That’s $1,440 a year. Switch to a therapeutic alternative for $15/month. You save $1,260. That’s a vacation. A new pair of shoes. A full tank of gas. Or just peace of mind.
And it’s not just about money. When people can afford their meds, they take them. A 2024 Healthgrades report showed that patients who switched to lower-cost alternatives were 40% more likely to take their pills every day. That means fewer ER visits. Fewer hospital stays. Better health.
Health systems are catching on. Epic and Cerner, the two biggest electronic health record systems, now have built-in tools that suggest therapeutic alternatives at the point of prescribing. In 2024, one hospital system saw a 15.3% increase in these switches after adding the tool.
But until that’s everywhere, you have to ask. Your doctor can’t read your mind. They don’t know your budget unless you tell them.
Final Checklist: What to Do Today
Here’s your action plan:
- Look up your current meds. Use GoodRx. Find the lowest price at a nearby pharmacy.
- Find alternatives. Search for other drugs in the same class. For example: if you’re on Pravastatin, search for “statins” and compare.
- Check for coupons. Go to the drug manufacturer’s website. Look for patient assistance programs.
- Write down 1-2 options. Example: “Can I switch from Brilinta to Plavix? Plavix is $12/month.”
- Bring it to your next appointment. Say: “I’ve been researching cheaper options. Can we talk about switching?”
You’re not asking for a favor. You’re asking for smart, evidence-based care. And you deserve it.
Can I switch to a therapeutic alternative without my doctor’s approval?
No. Even if a drug looks cheaper, you can’t legally switch without your prescriber’s order. Pharmacists can’t substitute therapeutic alternatives without a new prescription. Always consult your doctor first.
Are therapeutic alternatives as safe as my current drug?
Yes-if they’re chosen correctly. The American College of Physicians requires that therapeutic alternatives have equivalent efficacy, similar safety profiles, and comparable dosing. Studies show that for most common conditions like hypertension, diabetes, and depression, outcomes are identical. But individual responses vary. That’s why a trial period is often recommended.
What if my insurance won’t cover the alternative?
Your doctor can file a “tiering exception” with your insurer. For Medicare Part D, this must be decided within 72 hours for urgent cases. Many private insurers also have fast-track processes. Bring documentation of cost and medical necessity to support your request.
Can I use GoodRx if I have Medicare?
Yes, but not at the same time as your insurance. You can use GoodRx instead of your insurance, but not alongside it. Compare the GoodRx price with your Medicare copay. If GoodRx is cheaper, pay cash. Many seniors do this for medications not covered well by Part D.
How long does it take to get a therapeutic alternative approved?
If your doctor agrees, you can get a new prescription the same day. Filing an insurance exception takes 1-14 days, depending on urgency. For urgent cases (like risk of hospitalization), Medicare requires a decision within 72 hours. Always ask your provider to mark the request as “urgent” if needed.