When you pick up a prescription, you might see two options: the familiar brand name or a cheaper generic. It’s tempting to assume they’re exactly the same. After all, the FDA says they are. But if you’ve been on medication for years-especially for something like high blood pressure, epilepsy, or thyroid disease-you might have noticed something odd. One version works. The other doesn’t. Or worse, it makes things worse.
What Does ‘Therapeutic Equivalence’ Really Mean?
The FDA requires generics to prove they’re bioequivalent to the brand-name drug. That means the amount of active ingredient absorbed into your bloodstream has to fall within 80-125% of the brand’s absorption rate. Sounds strict, right? But here’s the catch: that’s a 45% range. For most drugs, that’s fine. But for drugs with a narrow therapeutic index-like warfarin, levothyroxine, or phenytoin-tiny differences in absorption can mean the difference between control and crisis. A 2017 study found that patients switching from Synthroid (brand levothyroxine) to generic versions had a 12.3% higher chance of abnormal thyroid-stimulating hormone (TSH) levels. That’s not a glitch. That’s a clinically meaningful shift. Your body doesn’t care if the pill is labeled “Letrozole” or “Letrozole Generic.” It only cares if the dose is right. And sometimes, it isn’t.The Austrian Study That Changed the Conversation
In 2020, researchers analyzed data from nearly every person in Austria on chronic medication between 2007 and 2012. They looked at 17 different drugs, including antihypertensives, diabetes meds, and cholesterol drugs. The results were shocking. For patients taking brand-name blood pressure medications, the death rate was 53.8 per 1,000 patient-years. For those on generics? Just 30.2. That’s nearly half. Major cardiac events-heart attacks, strokes-were 83.6 per 1,000 for brand users, but only 51.3 for generic users. The study didn’t just compare pills. It tracked real outcomes: hospitalizations, survival rates, long-term complications. And the kicker? The advantage for generics held up even after adjusting for age, income, previous health history, and whether patients stopped taking the drug. The researchers didn’t find a flaw in the generics. They found the brand names were less safe. This wasn’t an accident. It wasn’t bias. It was a massive, real-world dataset tracking people over five years. And it suggested that, at least for some medications, generics might be the safer choice.But Then There Are the Cases That Don’t Fit
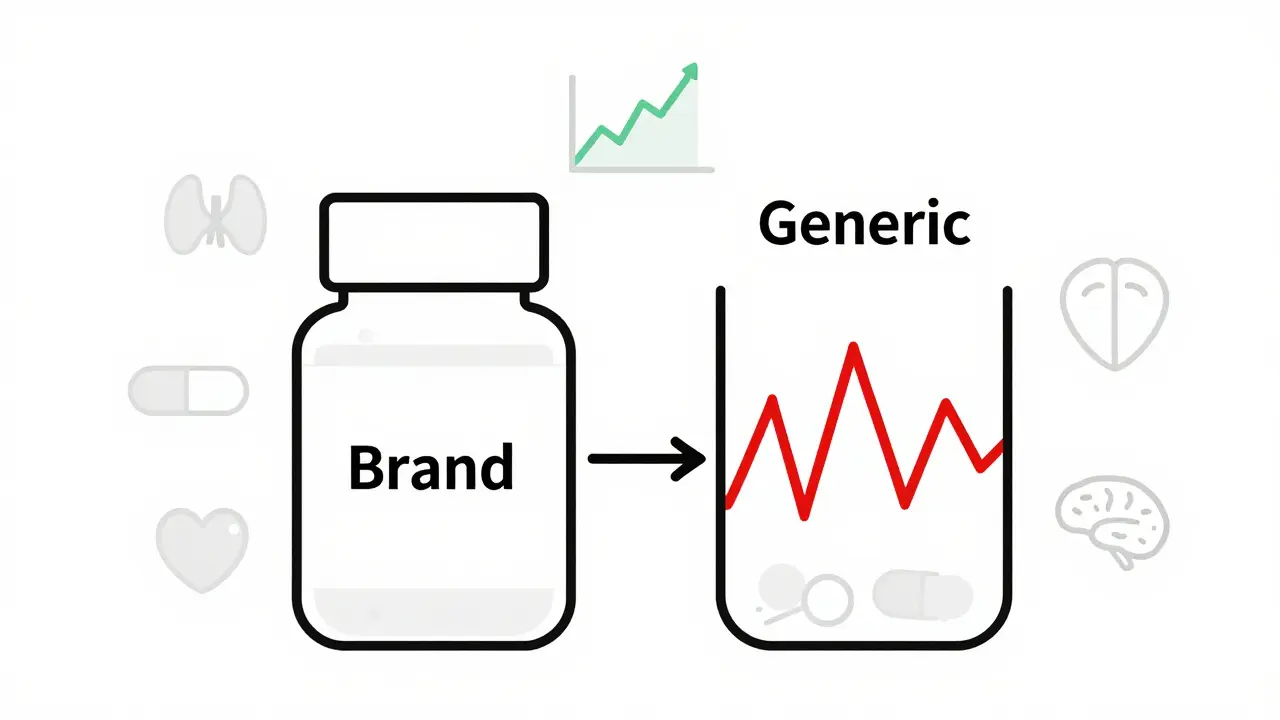
Science doesn’t always give one answer. Some patients report dramatic drops in effectiveness after switching. One case documented in the PMC database involved a man on generic ciprofloxacin. He kept getting infections. His fever stayed high. He felt worse. When he switched back to the brand-name Ciproxin, his symptoms vanished in days. Another patient on generic levofloxacin saw no improvement until he went back to Tavanic. These aren’t outliers. They’re real people with real suffering. A 2013 analysis of similar cases found that about 30% of patients saw improvement after switching back to brand drugs. Another 30% saw no change. And 30% got worse-either from side effects or because the generic simply didn’t work. Why? It’s not just the active ingredient. It’s the fillers. The coatings. The manufacturing process. A pill might have the same chemical in it, but if the tablet breaks down too slowly-or too fast-in your stomach, your body gets a different dose over time. For someone on a tight therapeutic window, that’s enough to trigger a seizure, a clot, or a thyroid crash.
Who’s Making Your Generic Drug?
Here’s something most people don’t know: the same brand-name company often makes the generic version too. These are called authorized generics. They’re identical to the brand-same factory, same formula, same packaging, just a different label. A 2018 analysis of adverse event reports showed something surprising. For amlodipine (a blood pressure drug), 56% of reports came from generic versions. But only 14% came from authorized generics. The brand version? 29.5%. That suggests the problem isn’t “generic vs brand.” It’s “this manufacturer vs that manufacturer.” A 2018 Ohio State University study dug deeper. They compared generic drugs made in the U.S. to those made in India. The Indian-made versions had a 54% higher rate of severe adverse events-hospitalizations, disabilities, even deaths. For ciprofloxacin, the difference was even starker: 62% higher hospitalization rates. This isn’t about quality control. It’s about oversight. The FDA inspects only a small fraction of overseas facilities. And when a pill is made in a factory 8,000 miles away, with different regulations, different standards, and less transparency, the risk goes up.What About the Big Studies That Say It’s Fine?
You’ll hear that generics are just as safe. And you’re right-most of the time, they are. A Harvard study tracked over 136,000 older adults on three blood pressure drugs after generics hit the market. No increase in ER visits or hospitalizations. That’s reassuring. But here’s what they didn’t measure: mild side effects. Fatigue. Dizziness. Brain fog. Changes in mood. These don’t land you in the hospital, but they can wreck your quality of life. And then there’s the data from PatientsLikeMe. Out of nearly 4,000 people on hypertension meds, 78% said generics worked just as well. But 13% said they were less effective. And 9% said they felt better on generics. That’s not a flat line. That’s a spectrum. The FDA’s own database, FAERS, shows over 1,200 reports between 2018 and 2022 saying “generic drug ineffective.” Compare that to 289 for brand-name drugs. That’s not because generics are bad. It’s because 92% of prescriptions are generic. More people = more reports. But the pattern still matters.
When You Should Be Careful
Not all drugs are created equal. Some need extra caution:- Levothyroxine - Even small changes in absorption can throw off your metabolism. Many endocrinologists still recommend brand-name Synthroid for stability.
- Warfarin - A 5% change in absorption can mean a dangerous clot or a bleed. INR levels must be rock steady.
- Lamotrigine - Used for epilepsy and bipolar disorder. Multiple patient reports on Reddit describe sudden seizure spikes after switching to generic.
- Anti-seizure drugs - Phenytoin, carbamazepine, valproate. All have narrow therapeutic windows.
- Inhalers and topical drugs - Bioequivalence testing is harder here. The delivery system matters as much as the drug.
What Should You Do?
The truth is, there’s no one-size-fits-all answer. For most people, generics are safe, effective, and save hundreds a year. But for others, the difference is life-changing. Here’s what works:- Stick with the same manufacturer if you’re stable. If your generic works, don’t switch unless you have to.
- Check the pill’s imprint. Generic manufacturers change frequently. If your pill looks different, ask why.
- Track your symptoms. Note changes in energy, mood, sleep, or side effects after a switch.
- For critical medications, ask your doctor for a “dispense as written” prescription. That blocks automatic substitution.
- If you feel worse after switching, don’t wait. Go back to the previous version. Document it. Tell your doctor.
Kristen Russell
Been on generic levothyroxine for 3 years and never had an issue. But I know people who switched and felt like zombies. Everyone’s body reacts differently.
Bryan Anderson
The data presented here is compelling, particularly the Austrian study. It underscores the importance of real-world outcomes over bioequivalence metrics alone. A nuanced understanding is essential.
sharad vyas
In my country, generics are the only option. People live. People survive. Maybe the problem is not the generic. Maybe the problem is we expect perfection from medicine.
Dusty Weeks
generic = bad 😡 brand = $$$ but works 🤷♂️ why do they even make generics if they’re just gonna mess with people??
Sally Denham-Vaughan
I had a friend switch from Synthroid to generic and her anxiety went through the roof. She cried for a week. Then switched back and felt like herself again. I don’t care what the FDA says - if you feel worse, don’t ignore it.
Bill Medley
The statistical variance in bioequivalence is concerning. For drugs with narrow therapeutic indices, the 80-125% range may be insufficient to ensure clinical consistency.
Richard Thomas
It’s fascinating how we reduce complex human physiology to a single metric - bioequivalence - as if the body is a test tube. The fillers, the coating, the dissolution rate, the manufacturing environment - these aren’t trivial. They’re part of the drug’s identity. And yet we treat them like packaging. For someone on warfarin, a 5% difference in absorption isn’t a statistical outlier - it’s a potential stroke. We’ve built a system that prioritizes cost over individual biological variability. That’s not efficiency. That’s negligence dressed up as progress.
Paul Ong
Stick with what works dont switch unless you have to and always check the pill imprint if it looks different ask your pharmacist dont just accept it
Andy Heinlein
My mom’s on generic cipro and kept getting UTIs. She switched back to brand and boom - no more infections. I’m telling you, if you feel off after switching, don’t brush it off. It’s not ‘all in your head’.
Ann Romine
I wonder how many of these generic manufacturers are owned by the same big pharma companies that make the brand versions. Maybe the real issue isn’t generic vs brand - it’s corporate control over supply chains.
Todd Nickel
The FDA’s bioequivalence standards are fundamentally flawed when applied to drugs with narrow therapeutic indices. The 80-125% window is mathematically sound for population-level averages, but it ignores the biological reality of individual pharmacokinetic variability. For a patient with epilepsy or thyroid disease, the difference between 80% and 125% isn’t a statistical curiosity - it’s a clinical precipice. The regulatory framework was designed for mass production, not precision medicine. Until we develop individualized dosing protocols or at least require batch-specific testing for critical medications, we’re gambling with people’s lives under the guise of cost-saving.
Austin Mac-Anabraba
Let’s be honest - if generics were truly equivalent, why do the same companies that make the brand drugs also make the generics? Because they know the difference. They’re profiting from your ignorance. The FDA is a puppet of Big Pharma. This isn’t science - it’s corporate theater.
Phoebe McKenzie
GENERIC DRUGS ARE A SCAM. THEY’RE MADE IN CHINA AND INDIA BY SLAVE LABOR AND THEY’RE KILLING AMERICANS. WHY ISN’T THE GOVERNMENT DOING SOMETHING? YOU PEOPLE ARE ALL SHEEP.
Stephen Gikuma
China’s making our pills and we’re letting it happen. This is economic warfare. The FDA doesn’t inspect factories overseas. They don’t even try. Our meds are being poisoned by foreign regimes. Wake up.
Bobby Collins
I think the government is hiding something. Why do so many people get worse on generics? Why do the same companies make both? I saw a video on TikTok that said the fillers in generics are laced with heavy metals. I don’t know if it’s true but… I’m scared.