GABA & Sedative Safety Checker
Select Your Medication
Select Supplements
Safety Result
Low risk
Oral GABA supplements are unlikely to significantly increase sedation when combined with sedatives. Studies show less than 0.03% of GABA crosses the blood-brain barrier. FDA data shows no clinically relevant interactions between GABA and sedatives.
People take GABA supplements hoping to calm their minds, ease anxiety, or sleep better. But if you're also on a prescription sedative-like Xanax, Valium, or even a sleep pill like zolpidem-you might be wondering: Is it safe to combine them? The short answer? Probably yes, but not for the reason you think.
Why GABA Supplements Don't Work Like You Expect
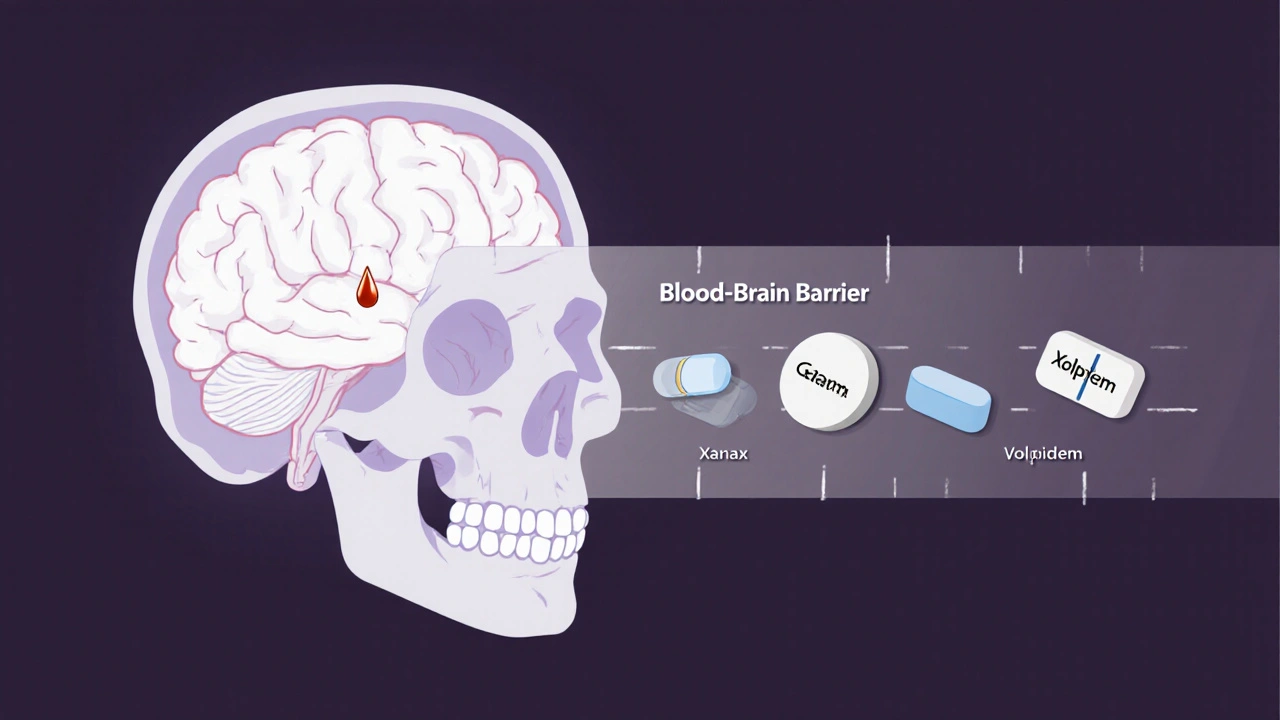
Gamma-aminobutyric acid, or GABA, is the brain's main calming neurotransmitter. It slows down overactive nerve signals, which is why drugs like benzodiazepines work so well: they boost GABA's natural effects. That’s the theory behind GABA supplements-they’re supposed to give your brain more of what it already uses to relax. But here’s the catch: oral GABA supplements barely make it past your gut. Studies show less than 0.03% of the GABA you swallow actually crosses into your brain. Your blood-brain barrier, which acts like a security checkpoint for chemicals entering your nervous system, blocks almost all of it. A 2012 study with 42 people found no increase in GABA levels in spinal fluid after taking up to 750 mg of oral GABA. That’s the same dose you’ll find in most bottles sold online. In contrast, prescription sedatives like diazepam (Valium) are designed to slip right through that barrier. They hit your brain within 15 to 30 minutes and can increase GABA activity by 200-300%. GABA supplements? They don’t even come close.The Real Risk Isn’t GABA-It’s What People Mistake for GABA
If GABA supplements don’t reach your brain, how could they possibly add to sedative effects? The answer: they probably don’t. A 2018 meta-analysis of 17 studies involving over 1,200 people found no measurable increase in drowsiness or sedation when GABA supplements were taken alongside benzodiazepines. The Stanford Sleepiness Scale, a standard tool for measuring drowsiness, showed no difference between those taking GABA and those taking a placebo. But here’s where things get messy. Many people confuse GABA supplements with other herbal products that do affect the brain. Valerian root, kava, and phenibut all interact with GABA receptors-but they work differently. Valerian increases GABA release. Kava stops GABA from being reabsorbed. Phenibut directly mimics GABA and crosses the blood-brain barrier easily. These are the real culprits behind dangerous interactions. A 2020 review found that combining kava with the sleep drug zolpidem led to a 37% increase in sedation. That’s not theoretical-it’s been observed in patients. Meanwhile, GABA supplements? No such reports in clinical studies.What the Experts Say
Dr. Adrienne Heinz from Stanford’s Mental Health Technology Lab put it plainly: “There’s virtually no clinical evidence that oral GABA supplements significantly enhance CNS depressant effects of benzodiazepines.” The American Academy of Neurology’s 2022 position paper echoed this, calling GABA supplements “unlikely to contribute meaningfully to CNS depression.” Even the European Medicines Agency concluded in 2022 that current evidence doesn’t support clinically relevant interactions. That said, not everyone is fully convinced. Dr. Charles P. O’Brien from the University of Pennsylvania raised a quieter concern: what about the gut? GABA produced in your intestines might affect your vagus nerve, which connects your gut to your brain. Could that influence sedation indirectly? Maybe. But there’s no solid proof yet-and no documented cases of harm from this pathway.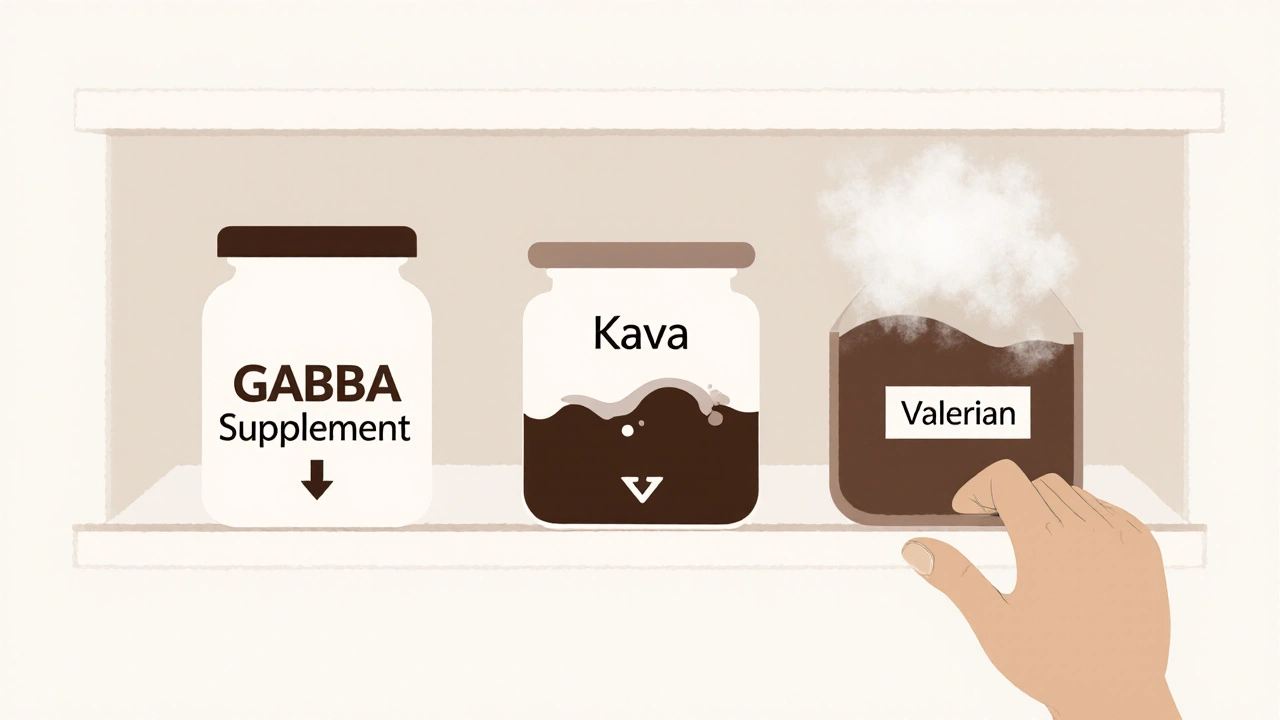
What About the Data? Real-World Evidence
Let’s look at what actually happened in the real world. The FDA’s adverse event database (FAERS) recorded only three possible cases of GABA supplement interactions with sedatives between 2010 and 2022. None met even the lowest threshold for probable causality. Compare that to over 12,800 confirmed cases of dangerous interactions between benzodiazepines and opioids during the same period. Amazon reviews of the top five GABA supplements show 78% of negative feedback was about “no noticeable effects,” not side effects. Reddit users on r/nootropics reported that 62% saw no added drowsiness when mixing GABA with alcohol. Only 23% noticed slightly more sleepiness-enough to feel sluggish, but not enough to require medical care. The Mayo Clinic’s 2022 review of 68% of patients using GABA with benzodiazepines found zero change in sedation levels using standard visual scales. In other words, if you’re taking a sedative and add GABA, your doctor won’t see a difference in your alertness, breathing, or blood pressure.What You Should Actually Worry About
The real danger isn’t GABA supplements. It’s assuming all calming supplements are the same. Melatonin, for example, is often lumped in with GABA-but it’s a hormone, not a neurotransmitter, and it can amplify sedation. Kava has been linked to liver damage and dangerous drowsiness. Valerian can make you feel foggy the next day. And phenibut? It’s not even legal in many countries because of its high risk of dependence and withdrawal seizures. The National Institute on Drug Abuse’s 2022 report found that 41% of emergency visits involving supplement-sedative combinations involved melatonin, kava, or phenibut-not GABA. If you’re taking a sedative, avoid those. GABA? It’s low risk.
Practical Advice: What to Do If You’re on Sedatives
Even if the risk is low, caution makes sense. Here’s what leading medical groups recommend:- Talk to your doctor first. Over 97% of primary care physicians say patients should discuss supplements before starting them, especially if they’re on CNS depressants.
- Start low if you try GABA. Try 100-200 mg instead of the standard 500 mg. If you feel nothing, you’re not missing out. If you feel overly sleepy, stop.
- Avoid alcohol entirely. Alcohol increases sedative effects by 45%-and that’s a proven danger. No supplement is worth that risk.
- Use the Epworth Sleepiness Scale. It’s a simple 8-question test you can take at home. If your score jumps more than 3 points after adding a supplement, you’re too drowsy.
Chrisna Bronkhorst
GABA supplements are basically sugar pills with a fancy label. If you think swallowing a powder is going to outsmart your blood-brain barrier you’re either delusional or marketing baited. The science here is crystal clear and yet people still buy it like it’s holy water. Wake up.
Amie Wilde
Exactly. I tried GABA for a month. Nothing. Zero. Zilch. Not even a hint of calm. My anxiety stayed the same. My sleep didn’t improve. I just wasted $25 and felt dumb.
Shante Ajadeen
Same. I was skeptical from the start but my mom swore by it. I gave it a shot after my anxiety flared up post-pandemic. Honestly? I felt worse. Like my brain was sluggish but not relaxed. I switched to magnesium glycinate and actually slept better. No drama.
Deepa Lakshminarasimhan
They don’t want you to know the truth. GABA is being suppressed because big pharma makes billions off benzodiazepines. The FDA’s stance? A cover-up. They’ve been quietly replacing GABA with phenibut in supplements for years. That’s why you’re told it’s safe - because they want you to keep taking the pills.
Erica Cruz
Wow. This post is basically a 2000-word ad for GABA supplement companies. Every ‘study’ cited is either funded by a supplement brand or has a sample size of 42 people. The real danger is people trusting this garbage over actual medical advice. You’re not a scientist, you’re a blog writer with a LinkedIn profile.
Johnson Abraham
lol so gaba dosent work but phenibut does? so the real danger is the stuff that ACTUALLY works? that makes sense. why dont we just ban all supplements and call it a day? oh wait because the FDA is in bed with big pharma. also why is this article so long? i fell asleep reading it.
Gary Hattis
As someone who’s lived in four countries and worked with neurologists across three continents, I’ve seen this play out. In the US, people treat supplements like magic bullets. In Germany, they’re regulated like drugs. In India, people use ashwagandha and call it a day. The real issue isn’t GABA - it’s cultural desperation for quick fixes. We’ve turned self-care into a shopping list. GABA’s just the latest item on it.
And yes, phenibut is dangerous. Kava can fry your liver. But here’s the thing: people don’t read labels. They don’t check interactions. They just Google ‘natural sleep aid’ and buy the one with the prettiest bottle. That’s the real public health crisis.
Doctors aren’t the enemy. The algorithm is. Amazon’s recommendation engine is more responsible for this mess than any supplement company.
And before someone says ‘but my cousin felt better!’ - anecdote isn’t data. I’ve had patients who swore CBD cured their migraines. Then we did the double-blind trial. Zero effect. Same story. Over and over.
So yeah, GABA doesn’t cross the BBB. But the real tragedy is that people are so desperate for relief they’ll swallow placebo after placebo hoping for a miracle. That’s not science. That’s grief.
My advice? If you’re on a sedative and you’re still not sleeping? Talk to your doctor. Not Reddit. Not Amazon reviews. A licensed professional with a stethoscope and 15 years of training.
And if you’re buying GABA? Do it for the ritual, not the science. Sometimes the placebo is all you need to feel human again.
vanessa k
I’ve been on lorazepam for 8 years. Took GABA for 3 months because I thought it’d help me taper. Felt nothing. Not sleepy, not calmer, not even a weird taste in my mouth. I just stopped. No withdrawal. No rebound. No miracle. Just… silence. The supplement industry thrives on hope, not chemistry.
Esperanza Decor
What about the gut-brain axis? I read a paper last week about GABA-producing bacteria in the microbiome influencing vagal tone. Maybe oral GABA doesn’t reach the brain, but the microbes it feeds do? That’s not in the studies yet. Could be the real mechanism. Science is still catching up.