Personal Eczema Trigger Tracker
Log Your Trigger Today
Environmental Triggers
Topical Triggers
Dietary Triggers
Emotional Triggers
Your Trigger History
Trigger Analysis
Your analysis will appear here based on the triggers you've logged.
When the skin starts to crawl, everyday tasks become a test of patience. Eczema is a chronic inflammatory condition that loves to turn ordinary skin into a battlefield of red, flaky patches and relentless Itch a sensation that triggers the urge to scratch, often worsening the rash. If you’re fed up with sleepless nights and constant discomfort, the good news is there are concrete steps you can take right now to calm the fire.
Key Takeaways
- Moisturize immediately after a bath to lock in water and protect the Skin barrier the outermost layer of skin that keeps irritants out and moisture in.
- Low‑strength Topical corticosteroid creams can quickly reduce inflammation when the itch spikes.
- Oral Antihistamine tablets are useful for nighttime itch and when allergens are the main trigger.
- Wet wrap therapy is a short‑term rescue method that hydrates skin and boosts medication absorption.
- Identify personal Trigger any factor that provokes a flare‑up, such as harsh soaps, temperature extremes, or stress and keep a simple log.
Why the Itch Happens
The sensation of itching in eczema isn’t random. When the skin’s protective Skin barrier is compromised, tiny cracks appear, allowing water to escape and irritants to slip in. The immune system reacts by releasing histamine and other inflammatory chemicals, which fire the nerve endings that tell your brain, “Scratch me!” This feedback loop is why a brief scratch often turns a mild patch into a weeping sore.
Step 1: Lock in Moisture with an Emollient
Think of an Emollient a thick, fragrance‑free cream or ointment designed to seal water into the skin as the first line of defense. Apply it within three minutes of stepping out of the shower while the skin is still damp. This timing creates a “molecular lock” that prevents evaporation.
- Choose products with ceramides, cholesterol, and fatty acids-these are the building blocks the barrier craves.
- Avoid lotions with alcohol, perfume, or dyes; they can irritate further.
- If you have very dry patches, a thin layer of petroleum‑based ointment (like white petrolatum) followed by a lighter cream works well.
Step 2: Use Targeted Medication When Itch Peaks
When a flare‑up pushes the itch beyond a manageable level, short‑term medication can break the cycle.
- Topical corticosteroid a cream or ointment that reduces inflammation by dampening the immune response-start with a low‑potency option (e.g., hydrocortisone 1%) for mild areas, and step up to medium‑potency (e.g., triamcinolone 0.1%) for thicker plaques. Apply a thin layer once or twice daily for no more than two weeks without a break.
- Oral Antihistamine a medication that blocks histamine receptors, reducing the itch sensation such as cetirizine or loratadine can be taken at night if the itch interferes with sleep. They’re not a substitute for topical steroids but work well together.
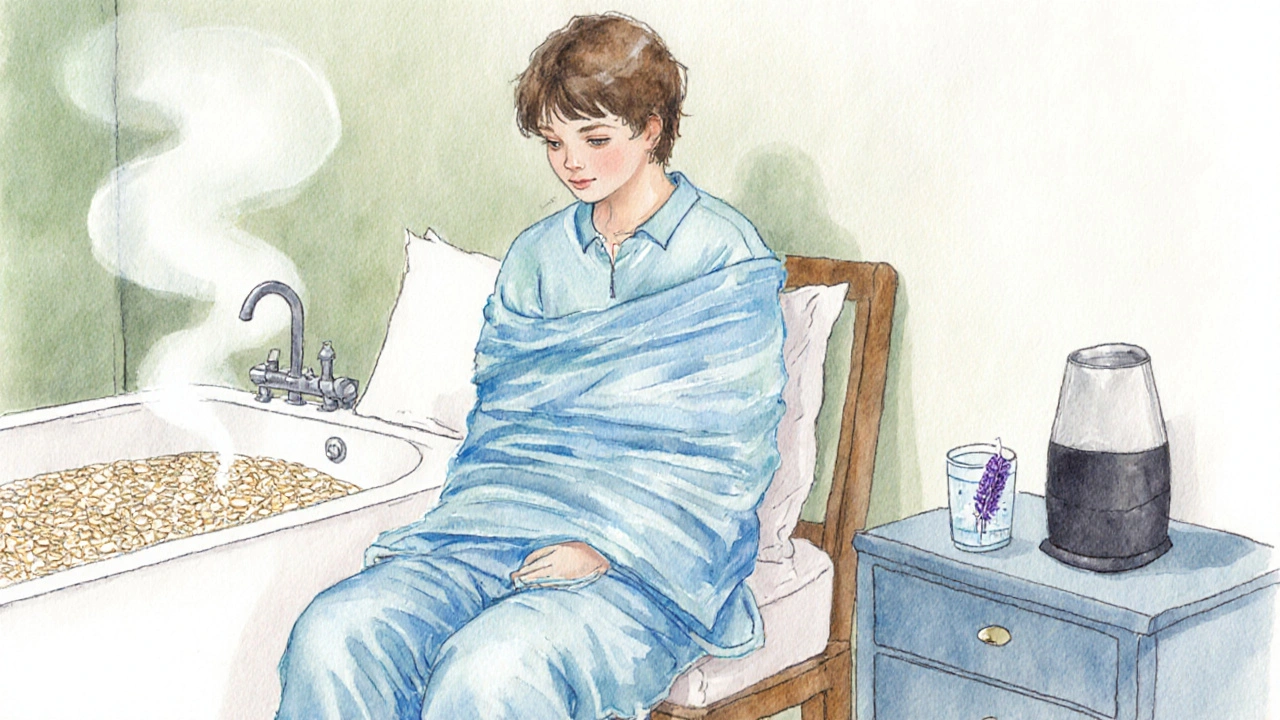
Step 3: Try Wet Wrap Therapy for a Quick Reset
Wet wrap therapy is a short, intensive approach often recommended for severe flares. Here’s how to do it safely at home:
- Take a lukewarm bath (no hotter than 98°F/37°C) for 10‑15 minutes. Add colloidal oatmeal or a gentle, fragrance‑free bath oil to soothe.
- Pat the skin dry, leaving it slightly damp, then slather a thin layer of a prescribed Topical corticosteroid over the affected patches.
- Cover the area with a long‑sleeve cotton shirt and long pants that are still wet from the bath.
- Layer a dry, breathable garment (like a cotton T‑shirt) over the wet clothing.
- Leave the wraps on for 2‑4 hours, then remove, shower gently, and re‑apply your regular emollient.
Do this once daily for up to three days. If you notice increased redness or signs of infection, stop and consult a clinician.
Step 4: Spot and Avoid Your Personal Triggers
Everyone’s eczema triggers are a little different, but most fall into a few classic categories. Keep a simple diary for two weeks: note the weather, foods, soaps, and stress levels alongside flare intensity.
- Environmental: dry air, sudden temperature changes, pollen, pet dander.
- Topical: harsh soaps, wool or synthetic fabrics, scented lotions.
- Dietary: dairy, eggs, nuts, or gluten can aggravate some people-eliminate one at a time to test.
- Emotional: anxiety and lack of sleep are known to heighten itch perception.
When a trigger is identified, replace it with a gentler alternative. For example, swap a regular body wash for a fragrance‑free, pH‑balanced cleanser, and opt for 100% cotton sleepwear.
Step 5: Lifestyle Tweaks that Keep Itch at Bay
- Cool compresses: A damp, cool washcloth applied for 5 minutes can calm hot, itchy spots without medication.
- Short nails: Keeping fingernails trimmed reduces the risk of skin damage if you do scratch.
- Humidifier: Running a cool‑mist humidifier at night adds moisture to the air, helping the skin stay hydrated.
- Stress management: Simple breathing exercises or a short walk can lower cortisol, which in turn reduces itch intensity.
Quick Comparison of Common Itch‑Control Options
| Option | Mechanism | Typical Use‑Case | Potential Side Effects |
|---|---|---|---|
| Emollient | Seals moisture, repairs barrier | Daily maintenance, after baths | Rare irritation if fragrance present |
| Low‑potency Topical corticosteroid | Suppresses local immune response | Mild flare‑ups, short‑term | Skin thinning with prolonged use |
| Oral Antihistamine | Blocks histamine‑driven itch signals | Nighttime itch, allergy‑related spikes | Drowsiness (non‑sedating options available) |
| Wet wrap therapy | Hydrates skin, enhances medication absorption | Severe flares, short‑term rescue | Heat, temporary skin maceration |
Frequently Asked Questions
How often should I apply moisturizer?
Apply a liberal amount within three minutes of bathing, then re‑apply whenever your skin feels tight or after washing your hands.
Can I use over‑the‑counter hydrocortisone on my face?
Yes, but only a thin layer and for a maximum of one week. If redness persists, seek a dermatologist’s advice.
Why does my eczema get worse in winter?
Cold, dry air strips moisture from the skin, weakening the barrier and triggering itch. Using a humidifier and a richer ointment can offset the effect.
Are there natural remedies that actually work?
Colloidal oatmeal baths, coconut oil applied after a shower, and plain aloe vera gel have modest soothing benefits. They should complement, not replace, medically proven treatments.
When should I see a doctor for my eczema itch?
If the itch interferes with sleep, if you notice signs of infection (pus, increasing redness, fever), or if over‑the‑counter options fail after two weeks, schedule a visit.
Next Steps and Troubleshooting
If you’ve tried the steps above and the itch still dominates your day, consider these adjustments:
- Prescription options: A dermatologist may recommend a higher‑potency steroid, a calcineurin inhibitor (e.g., tacrolimus), or phototherapy.
- Allergy testing: Identifying hidden food or environmental allergens can uncover a hidden trigger.
- Psychological support: Chronic itch can cause anxiety; cognitive‑behavioral therapy has helped many patients break the itch‑scratch cycle.
Remember, eczema management is a marathon, not a sprint. Consistency with moisturizers, a clear plan for flare‑ups, and a proactive eye on triggers together create the eczema itch relief you’ve been looking for.

Brett Coombs
They don’t want us to know that moisturizers are just a market scam.
John Hoffmann
The article outlines a sensible regimen, yet it omits the necessity of patch‑testing new emollients before widespread use. Consistency in application, ideally within three minutes post‑bath, maximises barrier repair. Moreover, the recommendation to avoid fragrance is well‑founded, as volatile compounds frequently exacerbate pruritus.
Amit Kumar
Hey everyone! 😊 I just wanted to say how great it feels to see such a thorough guide on eczema itch relief. 🌟 First, remember that the skin barrier is like a fortress; keeping it reinforced with thick, fragrance‑free emollients is key.
Second, don’t underestimate the power of a consistent routine – apply moisturizer right after you shower, while the skin is still damp, to lock in that precious moisture.
Third, if you’re dealing with a flare, a short course of a low‑potency steroid can calm inflammation fast, but always follow the doctor’s instructions and don’t overuse it.
Fourth, the cool compress trick is a lifesaver; a damp washcloth for a few minutes can instantly soothe that burning itch without any meds.
Fifth, using a humidifier at night adds ambient moisture to the air, which can dramatically reduce nighttime itching.
Sixth, keep your nails trimmed – a short nail reduces the chance of skin damage when you inevitably scratch.
Seventh, think about your clothing choices: soft, breathable cotton is your friend, while wool and synthetics can irritate sensitive skin.
Eighth, stress management is underrated; simple breathing exercises or a short walk can lower cortisol, which in turn can lessen itch intensity.
Ninth, keep a simple diary for two weeks, noting foods, weather, and stressors alongside flare severity – patterns will emerge faster than you think.
Tenth, consider trying wet‑wrap therapy for severe flares – it hydrates, enhances medication absorption, and gives a quick reset.
Eleventh, if you suspect dietary triggers, eliminate one potential culprit at a time (like dairy or nuts) and observe any changes.
Twelfth, always stay hydrated – drinking enough water supports overall skin health from the inside out.
Thirteenth, if over‑the‑counter options don’t help after two weeks, seek a dermatologist for prescription‑strength options or phototherapy.
Fourteenth, remember that eczema is a marathon, not a sprint; consistency and patience are your greatest allies.
Finally, celebrate every small victory – a night of uninterrupted sleep or a day with reduced redness is progress! Keep sharing your experiences, and let’s support each other on this journey. 🌈
Mustapha Mustapha
Good points all around. I’d add that a simple humidifier at night can make a noticeable difference, especially in dry climates. Also, keep your bedroom temperature moderate; extreme heat or cold often aggravates the itch.
Ben Muncie
Using over‑the‑counter steroids without medical guidance is irresponsible; people should consult a professional before self‑medicating.
Greg DiMedio
Wow, another “miracle cure” list. As if slathering on creams is going to fix everything. Maybe try a bit of common sense before jumping on every trendy tip.
Kara Guilbert
Honestly, if you dont read the labels carefully you could end up with worse rash. Theres alot more to it than just applying any old lotion.
Sonia Michelle
From a philosophical standpoint, eczema reminds us that our bodies are in constant dialogue with the environment. Respecting that conversation-by listening to triggers, honoring the skin’s needs, and responding with mindful care-can transform suffering into a practice of self‑awareness.
Neil Collette
Oh great, another “step‑by‑step” guide that pretends to be revolutionary! As if you’ve never heard of moisturizers before. The real issue is that most people are too lazy to follow any of these “simple” instructions, so they keep scratching like idiots. And let’s not forget the endless market hype pushing overpriced creams that barely do anything. Seriously, if you’re not willing to commit, no amount of wet‑wraps or fancy tables will save you.
joshua Dangerfield
I hear you, Neil, and I get why you’re frustrated. It’s true that many skip the basics, but some folks actually do need a clear roadmap. Maybe we can bridge the gap: encourage people to start with the simplest steps-like a good moisturizer-and then move on to the more involved methods if needed.
Abhimanyu Singh Rathore
Indeed, consistency is paramount; applying emollient within three minutes post‑shower creates a “molecular lock” - a term that, while colloquial, effectively conveys the barrier‑repair process. Moreover, avoiding fragrances, alcohol, and dyes is non‑negotiable; these additives often exacerbate pruritus, leading to a vicious itch‑scratch cycle.
Stephen Lewis
To expand upon the previous point, it is advisable to select products containing ceramides, cholesterol, and fatty acids, as these constituents are integral to the restoration of epidermal integrity. Accordingly, a disciplined regimen, coupled with vigilant monitoring for adverse reactions, will facilitate optimal therapeutic outcomes.
janvi patel
I think the whole “dry skin equals eczema” narrative is over‑simplified; there are deeper immunological factors at play.
Adele Joablife
While it’s true that immunological mechanisms are significant, disregarding the practical steps-like barrier repair and trigger avoidance-undermines a holistic approach. Effective management requires both scientific understanding and diligent daily care.