People assume generic drugs are just cheaper copies of brand-name meds. And for the most part, they’re right. But when it comes to drug interactions, something strange happens. Patients swear their generic version causes new side effects or stops working - even though the active ingredient is identical. What’s really going on?
Why Do People Think Generics Interact Differently?
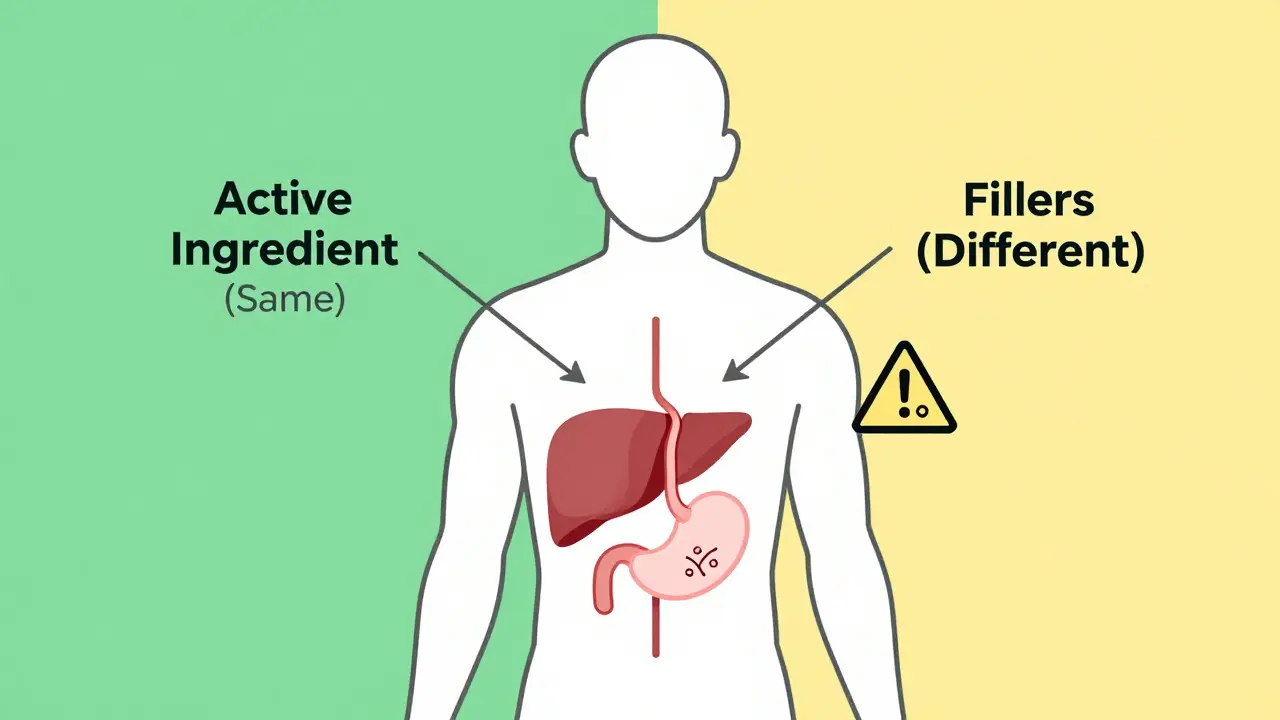
The short answer: they don’t. Not pharmacologically. The FDA requires every generic drug to contain the same active ingredient, in the same strength, and delivered the same way as the brand-name version. That means if your brand-name statin interacts with grapefruit juice, so does the generic. If your brand-name blood thinner reacts with vitamin K-rich foods, so does the generic. So why do so many patients report problems? It’s not the drug. It’s the filler. Generic manufacturers use different inactive ingredients - things like lactose, dyes, preservatives, or binders - to keep costs low. These don’t affect how the medicine works in your body. But for some people, they trigger reactions. One patient in 2021 had stomach cramps after switching to a generic levothyroxine. The brand version used cornstarch. The generic used lactose. She was lactose intolerant. The drug worked fine. The filler didn’t. Then there’s the nocebo effect. If you believe generics are inferior, your brain can make you feel worse. A 2022 Kaiser Family Foundation survey found nearly half of patients thought generics worked differently. But when researchers checked medical records, only 3.7% of those reports matched actual physiological changes.What Actually Causes Drug Interactions?
Drug interactions happen because of how your body processes the active ingredient. There are three real types:- Drug-drug interactions: Like fluconazole (an antifungal) making simvastatin (a cholesterol drug) build up to dangerous levels - 300-400% higher. This happens whether the simvastatin is brand or generic.
- Drug-food interactions: Grapefruit juice blocks an enzyme (CYP3A4) that breaks down many drugs. It can spike blood levels of blood pressure meds, statins, or immunosuppressants by up to 70%. Again, doesn’t matter if it’s generic.
- Drug-condition interactions: Diphenhydramine (Benadryl) can raise eye pressure. That’s risky if you have glaucoma. The same risk applies to every version of the drug.
The Real Problem: Switching Between Generics
Here’s where things get messy. You might get one generic this month - made by Company A. Next month, your pharmacy switches you to a different generic - made by Company B. Both are FDA-approved. Both have the same active ingredient. But they use different fillers. In 2022, IQVIA found that 32% of U.S. prescriptions switched between generic manufacturers within a year. For most people, this is invisible. But for patients on drugs with a narrow therapeutic index - where tiny changes in blood levels can cause harm - it matters. Drugs like warfarin, levothyroxine, digoxin, and phenytoin fall into this category. A 10% shift in warfarin levels can mean the difference between a clot and a stroke. The FDA requires tighter bioequivalence standards for these drugs (90-112% instead of 80-125%). But even then, switching between manufacturers can cause confusion. A 2023 review on Inspire.com looked at 112 reports of warfarin generics causing INR fluctuations. Pharmacists followed up. 89% of those cases were traced to dietary changes - eating more spinach, skipping meals, drinking alcohol - not the generic.Who’s at Risk?
Not everyone. But certain groups need extra care:- Patients on narrow therapeutic index drugs: Stick with the same generic manufacturer if possible. Hospitals often do this by design - 76% of U.S. hospitals use one preferred generic for critical drugs like warfarin.
- People with food allergies or sensitivities: Lactose, gluten, or artificial colors in fillers can cause real symptoms. Check the label. If you’re unsure, ask your pharmacist.
- Older adults on multiple medications: Polypharmacy increases interaction risk. A generic switch might seem harmless, but if it changes absorption timing, it could throw off your whole regimen.
- Patients who’ve had bad experiences before: If you had a reaction to a generic once, don’t assume it’ll happen again. But do tell your pharmacist. They can track which manufacturer you tolerate best.
What Should You Do?
You don’t need to avoid generics. They’re safe, effective, and save billions. But be smart:- Ask your pharmacist: "Which manufacturer makes this generic?" Write it down. If you switch and feel different, you’ll know why.
- Don’t assume a new generic is "worse." If you feel off, check your diet, sleep, alcohol intake, or other meds first.
- If you’re on warfarin, levothyroxine, or similar drugs, request consistency. Most pharmacies will honor it if you ask.
- Read the patient information sheet. It lists all ingredients - even the fillers. If you see something you’re allergic to, speak up.
- Report unusual symptoms to your doctor and the FDA’s MedWatch program. Most reports are harmless. But tracking them helps catch rare issues.
The Bigger Picture
Generics make up 90% of all prescriptions in the U.S. They’ve saved the healthcare system over $300 billion in the last decade. But misconceptions cost money - and lives. A 2023 Health Affairs study found that 1.2 million people unnecessarily pay for brand-name drugs each year because they fear generics interact differently. That’s $8.7 billion wasted. The FDA’s 2024 Generics Awareness Campaign is trying to fix this. They’re funding patient education, training pharmacists, and using AI to track real-world interaction data across 12.7 million prescriptions. The science is clear: generics don’t interact differently. The active ingredient controls that. But the system is messy. Pharmacies switch suppliers. Patients get confused. Labels are hard to read. Your job? Stay informed. Ask questions. Don’t let fear stop you from saving money - but don’t ignore your body either. If something feels off, it’s not the generic. It’s something else. And you’re the best person to notice it.What to Do If You Think Your Generic Isn’t Working
If you’ve switched to a generic and feel different - more tired, more anxious, less effective - don’t panic. Don’t stop taking it. Don’t assume it’s the drug. Do this instead:- Check your pill. Is it a different color or shape? That’s a sign you got a new manufacturer.
- Review your diet. Did you start eating more leafy greens? More grapefruit? Less protein?
- Check other meds. Did your doctor add or change anything else?
- Call your pharmacist. Ask: "Is this the same manufacturer as last time?"
- If nothing changed, and you still feel off - get a blood test. For warfarin, that’s INR. For thyroid meds, it’s TSH. Numbers don’t lie.
Are generic drugs less safe than brand-name drugs?
No. Generic drugs must meet the same FDA standards as brand-name drugs for safety, strength, quality, and performance. The active ingredient is identical. The only differences are in inactive ingredients like fillers or dyes, which rarely cause issues. Over 97% of generics show bioequivalence within strict limits, and adverse events linked to generics are extremely rare.
Can generic drugs cause different side effects than brand-name drugs?
They can - but not because of the active ingredient. Side effects from fillers like lactose, gluten, or artificial colors can occur in sensitive individuals. For example, a patient allergic to lactose might get stomach upset from a generic levothyroxine that uses it, while the brand version uses cornstarch. These are not drug interactions - they’re ingredient reactions. Always check the inactive ingredients list on the label.
Why do some people say their generic medication doesn’t work as well?
This is often the nocebo effect - when expecting a drug to be less effective leads to feeling like it is. Studies show patients report more side effects or reduced effectiveness with generics, even when blood levels and clinical outcomes are identical to brand-name versions. Psychological factors, packaging differences, or previous bad experiences can all contribute. In real-world data, only about 13% of reported differences are pharmacologically real.
Should I stick with one generic manufacturer for my medication?
For drugs with a narrow therapeutic index - like warfarin, levothyroxine, or phenytoin - yes. Even small changes in absorption due to different fillers can affect blood levels. If you’re on one of these, ask your pharmacist to keep you on the same manufacturer. Most pharmacies can do this if you request it. For most other medications, switching is fine.
How do I know if my generic drug has different ingredients?
Look at the patient information leaflet inside the pill bottle. It lists all active and inactive ingredients. If you’re unsure, ask your pharmacist to compare the label with your previous prescription. You can also check the FDA’s Orange Book online (though not linked here) to see approved generics and their manufacturers. Don’t rely on pill color or shape - those can change even within the same manufacturer.
Paul Huppert
Had this happen with my thyroid med. Switched generics, started feeling like a zombie. Turned out the new one had lactose. I’m lactose intolerant. Didn’t even think to check the label until my stomach screamed at me.
Hanna Spittel
LOL the FDA is just in bed with Big Pharma 😏 They want you to think generics are ‘the same’ so you don’t ask questions. But ask any pharmacist who’s been around 20 years-they’ll tell you some generics are total garbage.
Darren Pearson
It’s not merely a matter of filler ingredients-it’s the bioavailability variance within the FDA’s permissive 80–125% window. For drugs with narrow therapeutic indices, even a 10% shift can precipitate clinically significant deviations. The regulatory framework is structurally inadequate for precision medicine.
Stewart Smith
So you’re telling me my brain is the problem? Cool. So when I feel like I’m slowly turning into a zombie after switching generics… it’s just my imagination? 😌
Frank SSS
Man I used to be one of those guys who swore generics were trash. Then I got on warfarin. Switched from one generic to another, INR went from 2.3 to 4.8 in three days. Turned out the new one had a different binder that slowed absorption. Didn’t have a clue until my doctor said ‘you didn’t change your diet, did you?’ Nope. Just the pill. Now I ask for the brand every time. Worth it.
And yeah, I know the science says it’s fine. But my body doesn’t read FDA reports. It reads the pill in my hand.
Also, why do all the generics look like they were designed by a 12-year-old with a crayon? I can’t tell them apart.
And don’t get me started on the time I got a generic that had a weird chalky taste. I thought I was going to throw up. Turned out it had magnesium stearate. Never again.
My point? If you’re on something that keeps you alive, don’t gamble. Ask for consistency. Even if it’s a pain.
And yeah, I know I sound like a hypochondriac. But I’d rather be the guy who asks too many questions than the guy who ends up in the ER because ‘it’s just a filler’.
Also, the nocebo effect is real-but so is the placebo effect. And if my brain thinks the pill’s gonna kill me, it’s gonna feel like it is. That’s not all in my head. That’s my body listening.
Just sayin’.
Chandreson Chandreas
Life is about balance, man. The system’s broken? Yeah. But the answer isn’t to reject generics. It’s to demand transparency. Ask for the label. Know your filler. Your body’s not your enemy-it’s your map. Just learn to read it.
And hey, if you’re stressed about it? Breathe. Medication’s just one part of the puzzle. Sleep. Water. Movement. That stuff matters more than you think.
Retha Dungga
they say the active ingredient is the same but what if the filler is the real drug and the active ingredient is just decoration 🤔
Kayla Kliphardt
I just read the patient leaflet for the first time after reading this. Turns out my generic metformin has FD&C Yellow No. 6. I’m allergic to that. No wonder I get hives. I’m calling my pharmacist tomorrow.
Jenny Salmingo
My grandma takes levothyroxine. She switched generics and started feeling cold all the time. We checked the label-new one had lactose. She’s been dairy-free since she was 6. She went back to the old one. Now she’s fine. Simple fix. No drama.
Branden Temew
So the system’s designed to save money… but the cost is your peace of mind? Classic. We optimize for efficiency, not humanity. Meanwhile, people are out here Googling ‘why do I feel like I’m dying after taking my pill’ because no one told them to check the dye.
Generics aren’t the enemy. The lack of education is.
Brady K.
Let me get this straight: the FDA mandates identical active ingredients, identical interaction warnings, identical bioequivalence standards for narrow-therapeutic-index drugs… but patients still panic because the pill is a different color? We’re not dealing with a pharmacology problem. We’re dealing with a psychological and systemic failure of communication. The real drug interaction is between fear and bureaucracy.
And don’t even get me started on how pharmacies switch suppliers like it’s a game of musical chairs. If you’re on warfarin and your pharmacy doesn’t offer manufacturer consistency on request, find a new pharmacy. That’s not paranoia. That’s basic risk management.
Also, if you’re still buying brand-name drugs because you think generics are ‘less safe’-you’re not saving money. You’re subsidizing corporate greed. And your pharmacist knows it.
Knowledge isn’t power here. It’s survival.
Brandon Boyd
Hey, if you’re worried about your meds, don’t stress-just take action. Ask your pharmacist. Check the label. Write down the manufacturer. Keep a little notebook. It’s not hard. You got this. Your health is worth the 2 minutes it takes to ask a question.
And hey-your body talks. Listen. If something feels off, it’s not ‘all in your head.’ It’s your body saying ‘hey, something changed.’ Don’t ignore it. But also don’t panic. Just investigate.
You’re not broken. You’re just awake. And that’s a good thing.
John Chapman
Bro I switched to a generic for my blood pressure med and my heart started racing. Thought I was having a panic attack. Turned out the new one had a different coating that made it dissolve faster. My BP spiked. Called my doc. Switched back. Done. Don’t let them tell you it’s ‘all in your head’ when your body’s screaming.