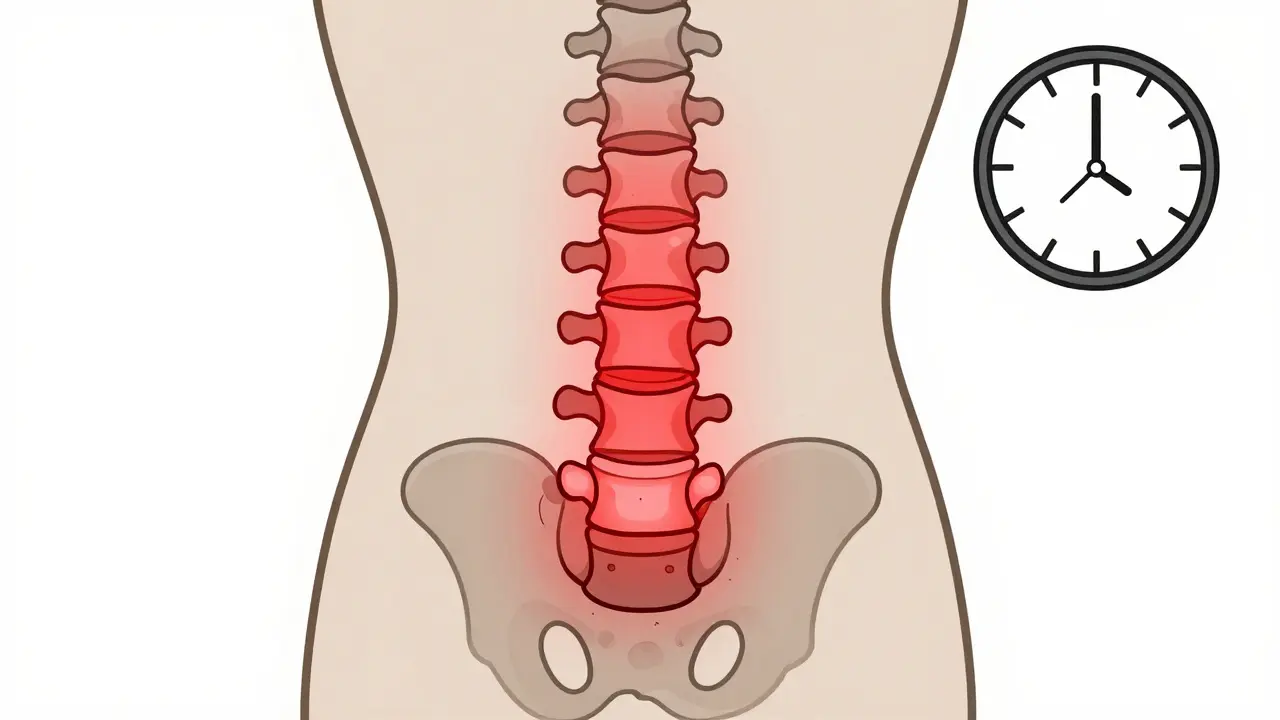
When your back pain doesn’t get better with rest-if it actually gets worse-and wakes you up in the early hours, it’s not just a bad night’s sleep. It could be ankylosing spondylitis, a chronic autoimmune condition that slowly fuses your spine. Unlike typical back pain from lifting something heavy or sitting too long, AS doesn’t fade with a massage or a day off. It’s inflammation that starts in the sacroiliac joints, creeps up the spine, and if left unchecked, can turn your vertebrae into a single rigid bone-what doctors call a "bamboo spine."
What Ankylosing Spondylitis Really Does to Your Body
Ankylosing spondylitis (AS) targets the entheses-the places where tendons and ligaments attach to bone. That’s why the pain often begins in the lower back and hips. Over time, the body tries to "repair" the inflamed tissue by growing new bone. These bony growths, called syndesmophytes, bridge the gaps between vertebrae. Eventually, they fuse. About 30-40% of people with AS develop this fusion within 10 to 20 years, according to the Cleveland Clinic.
The condition usually starts before age 45. Eight out of ten people first notice symptoms between 17 and 45. Men are two to three times more likely to be affected than women, though women often have milder symptoms and are diagnosed later. A strong genetic link exists: up to 96% of Caucasian patients carry the HLA-B27 gene, compared to just 6-8% of the general population. But having the gene doesn’t guarantee you’ll get AS-it just raises the risk.
It’s not just the spine. About one in three people with AS develop uveitis-an inflammation of the eye that causes redness, pain, and blurred vision. Up to half may also have inflammatory bowel disease, and about 1 in 10 develop psoriasis. These aren’t random side effects. They’re part of the same immune system malfunction.
How to Tell If It’s AS and Not Just Back Pain
Most people with AS are misdiagnosed for years. The average patient sees four doctors before getting the right answer. Why? Because the early signs look like ordinary back pain.
Here’s how to spot the difference:
- Duration: Pain lasts more than three months, not days or weeks.
- Timing: Worse in the morning, improves with movement. You might wake up stiff and unable to move for 30 minutes or more.
- Pattern: Pain wakes you up between 3 and 6 a.m. and improves after getting up.
- Response to rest: Rest makes it worse. Movement helps.
- Family history: A close relative with AS, psoriasis, or inflammatory bowel disease increases your risk.
Doctors use imaging to confirm. X-rays show bone changes, but only after damage has occurred. MRI can detect inflammation in the sacroiliac joints years before X-rays do. That’s why the 2022 ASAS-EULAR guidelines now recommend MRI as the first-line imaging tool for suspected AS.
Why Early Treatment Changes Everything
The biggest mistake people make is waiting. AS isn’t just about pain-it’s about losing your ability to move. Once bone fuses, it’s permanent. But if you catch it early, you can slow or even stop the damage.
First-line treatment is NSAIDs-medications like naproxen or celecoxib. A 2023 study from Johns Hopkins found that consistent NSAID use reduces radiographic progression by 50% over two years compared to taking them only when it hurts. That’s not just symptom relief-it’s disease modification.
If NSAIDs aren’t enough, biologics step in. TNF inhibitors like adalimumab (Humira) and etanercept (Enbrel) block the inflammatory protein driving the disease. In clinical trials, 40-60% of patients see a 40% or greater improvement in symptoms within 12 weeks. Newer drugs like secukinumab (Cosentyx), an IL-17 inhibitor, may reduce bone growth by 55% over two years. In 2023, the FDA approved upadacitinib (Rinvoq), a JAK inhibitor, after it showed a 45% response rate in patients who hadn’t responded to other treatments.
But these drugs aren’t cheap. Without insurance, biologics can cost $5,000 to $6,000 a month. Insurance coverage has improved, but prior authorizations and step therapy still delay access for many.

The Most Important Treatment: Movement
Medication alone isn’t enough. Physical therapy isn’t a bonus-it’s the core of treatment. A 2023 review from the Cleveland Clinic found that patients who stuck with daily exercise improved spinal mobility by 25-30% in just six months.
What works?
- Spinal extension exercises: Lie on your stomach and gently lift your chest off the floor. Hold for 5 seconds. Repeat 10 times. This fights the forward-curving posture AS causes.
- Deep breathing: AS can stiffen the rib cage, making it hard to breathe deeply. Practice inhaling slowly through your nose, expanding your ribs, then exhaling fully through your mouth. Do this 10 times daily.
- Aquatic therapy: Swimming or water aerobics reduces joint stress while letting you move freely. One patient on Reddit reported cutting morning stiffness from 90 minutes to 20 minutes after just three months of daily swimming.
- Posture training: Sit with your back straight, shoulders back. Sleep on a firm mattress without a pillow under your head. Use a lumbar roll when sitting for long periods.
Adherence is the biggest hurdle. Studies show only 45% of patients stick with exercise after one month. But with digital reminders and tracking apps, that number jumps to 78% by six months. The Spondylitis Association of America offers free online exercise videos. Johns Hopkins has AS-specific yoga routines designed for limited mobility.
Living With AS: Daily Strategies That Work
AS doesn’t just hurt your spine-it drains your energy. Seventy-four percent of patients say fatigue is their worst symptom. It’s not laziness. It’s inflammation affecting your entire body.
Here’s how to manage daily life:
- Start slow in the morning: Before getting out of bed, do gentle neck rolls, shoulder shrugs, and knee-to-chest stretches. Warm up your joints before standing.
- Use heat: A heating pad on your lower back for 20 minutes before exercise eases stiffness better than ice.
- Workplace adjustments: Standing desks, ergonomic chairs, and frequent movement breaks can cut pain by 35%. Many patients qualify for workplace accommodations under the ADA.
- Track your flare-ups: Keep a simple log: pain level (1-10), sleep quality, exercise done, medications taken. Patterns emerge over time, helping you avoid triggers.
One patient documented on HealthUnlocked how a personalized PT program kept her spine flexible for 15 years-even with HLA-B27 positivity. Her secret? Consistency. Not perfection. Some days she did 10 minutes. Other days, 45. But she never skipped for more than two days in a row.
What’s Next for AS Treatment?
The future is promising. The STABILITY trial, currently enrolling 500 patients across 35 U.S. centers, is testing whether 150 minutes of moderate-to-vigorous exercise per week-like brisk walking, cycling, or swimming-can prevent spinal fusion better than current recommendations. Early data suggests it can improve mobility by 30%.
JAK inhibitors like upadacitinib are gaining ground. By 2027, they could make up 25% of the AS treatment market, according to Evaluate Pharma. Digital health tools-apps that track posture, remind you to move, and connect you with physical therapists via video-are growing at 30% annually.
But the biggest breakthrough isn’t a drug. It’s awareness. More primary care doctors now recognize inflammatory back pain. More patients are finding support through groups like MySpondylitisTeam, where 8,321 members share tips, vent frustrations, and celebrate small wins.
Can You Live a Full Life With AS?
Yes. Twenty years ago, half of AS patients ended up disabled. Today, thanks to early diagnosis, better drugs, and consistent movement, 75% maintain functional independence. You might need to change how you lift groceries, how you sit at your desk, or how you exercise. But you don’t have to stop living.
The key isn’t finding a cure. It’s staying ahead of the disease. Take your meds. Move every day. Find your people. And don’t wait for pain to be unbearable before you act. The spine doesn’t heal itself. But with the right strategies, it doesn’t have to break you either.
Can ankylosing spondylitis be cured?
No, there is no cure for ankylosing spondylitis. But with early diagnosis and consistent treatment-including medication, physical therapy, and daily movement-most people can control symptoms, prevent spinal fusion, and live full, active lives. The goal isn’t to eliminate the disease, but to stop it from controlling your life.
Does ankylosing spondylitis get worse with age?
It can, but it doesn’t have to. Without treatment, inflammation leads to bone growth and fusion over time, often within 10-20 years. But with proper management-NSAIDs, biologics, and daily exercise-many people see little to no progression. The key is consistency. Skipping exercise or delaying medication increases the risk of permanent damage.
What exercises should I avoid with ankylosing spondylitis?
Avoid high-impact activities that jar the spine, like running on concrete or heavy weightlifting with poor form. Contact sports that risk spinal injury-football, rugby-are also not recommended. Instead, focus on low-impact, mobility-focused exercises: swimming, cycling, yoga designed for AS, and stretching. Always prioritize spinal extension and deep breathing over flexion movements.
How do I know if my AS is getting worse?
Watch for signs like increasing stiffness that doesn’t improve with movement, reduced ability to turn your head or bend backward, or difficulty taking deep breaths (which means your rib cage is stiffening). If your pain wakes you up more often, or you’re needing more NSAIDs just to get through the day, it’s time to talk to your rheumatologist. Regular imaging (MRI or X-ray) every 1-2 years helps track structural changes.
Is it safe to take biologics long-term?
Yes, for most people. Biologics have been used for over 20 years in AS, and long-term studies show they’re generally safe when monitored. The main risks are increased susceptibility to infections like tuberculosis or fungal infections. Before starting, you’ll be screened for TB and hepatitis. Regular check-ups and blood tests help catch issues early. The benefit-stopping spinal damage-usually outweighs the risks.
Can diet help with ankylosing spondylitis?
No diet can cure AS, but some people find that anti-inflammatory eating helps manage symptoms. Reducing processed sugars, refined carbs, and saturated fats may lower overall inflammation. Some report benefits from omega-3s (found in fish oil), turmeric, and avoiding nightshades (tomatoes, peppers, eggplant), though evidence is anecdotal. If you have IBD along with AS, a low-FODMAP or gluten-free diet may help digestive symptoms. Always talk to your doctor before making major dietary changes.
Ian Long
Been living with AS for 12 years. NSAIDs? Yeah, they help-but only if you take them like clockwork. I used to skip them on ‘good’ days. Big mistake. The pain didn’t come back-it just crept in slower until I couldn’t bend to tie my shoes. Now I take my naproxen like coffee. No excuses. And movement? I swim every morning. Water’s the only thing that lets me feel human again. Don’t wait until you’re fused to start.
Ashley Kronenwetter
Thank you for this comprehensive and clinically accurate overview. As a healthcare professional, I appreciate the emphasis on early MRI intervention and the distinction between mechanical and inflammatory back pain. The inclusion of recent 2023 guidelines and data from Johns Hopkins and Cleveland Clinic elevates this from anecdotal to evidence-based. A valuable resource for both patients and providers.
Heather Wilson
Let’s be real-this post reads like a pharmaceutical ad disguised as patient education. Biologics cost $6,000 a month? And you’re telling people to just ‘take them’? Meanwhile, the real solution-movement-is buried under 10 paragraphs of drug names. Also, ‘upadacitinib showed a 45% response rate’? 45% of who? People who didn’t respond to other drugs? That’s not a cure, that’s a consolation prize. And don’t get me started on the ‘anti-inflammatory diet’ nonsense. No diet changes your genetics. Wake up.
Micheal Murdoch
There’s a quiet revolution happening here, and most people don’t even see it. AS isn’t a death sentence-it’s a teacher. It forces you to listen to your body in a world that rewards ignoring it. The real win isn’t the MRI results or the drug regimen-it’s the person who wakes up stiff, does 10 minutes of stretching, and still shows up for their kid’s soccer game. That’s courage. That’s resilience. You don’t need a perfect routine. You just need to show up. Even if it’s messy. Even if it’s slow. Even if it’s just breathing deep for 30 seconds before you get out of bed. That’s the foundation. Everything else builds on that.
Chris Kauwe
Let me cut through the woke medical jargon. This isn’t ‘inflammatory back pain’-it’s a genetic weakness exploited by weak lifestyles. You think swimming and yoga fixes a broken spine? No. It’s the HLA-B27 gene. That’s the enemy. And if you’re not from a lineage that’s been tested for it, you’re just wasting time. We need genetic screening at 16, not after you’ve been misdiagnosed for 7 years. Stop glorifying ‘movement’ like it’s a spiritual practice. This is biology. Hard science. No fluff.
Matthew Maxwell
People who don’t take their meds or do their stretches are just lazy. If you’re too tired to do 10 minutes of exercise, you’re probably scrolling TikTok. This isn’t hard. It’s not expensive. It’s not complicated. You have a spine. You have a body. You have a choice: control it, or let it control you. The fact that 55% of people quit exercising after a month says everything about our culture’s decline. Weakness isn’t a medical condition-it’s a moral failure.
Kiruthiga Udayakumar
I have AS and I’m from India. We don’t have access to biologics here. No insurance. No Humira. But I swim in the local pond every morning, do back extensions on the floor, and drink turmeric milk. My pain? Down 70%. No fancy drugs. Just consistency. Don’t let rich-country medicine make you feel like you’re failing if you can’t afford it. Your body still hears you. Even in a village.
Patty Walters
just wanted to say the part about the heating pad before exercise? life changer. i used to ice everything bc that’s what the internet said. turned out heat is magic for as. also, the spondylitis association videos? saved me. no joke. i was about to quit PT until i found them. thanks for sharing that.
tali murah
Oh, so now we’re supposed to be grateful that we’re not ‘fully fused’ yet? That’s the bar? ‘You can still live a full life’-as long as you’re not a real person with real pain? You turned a lifelong, debilitating autoimmune disease into a motivational poster. ‘Just stretch more!’ Like that’s the solution. Meanwhile, I’m on three meds, in a wheelchair half the week, and you’re telling me to ‘find my people’ on MySpondylitisTeam? Thanks for the trauma porn.
Jenci Spradlin
so i’ve been doing the swimming thing for 8 months now. my doc said my xray looks better than last year’s. i didn’t think it was possible. also, i started using a dumb app called AS Tracker-it reminds me to move, logs my pain, and even has little badges. yeah, i know it sounds dumb. but it works. i didn’t skip for 3 days in a row since january. small wins, right? 🤘
Maggie Noe
the fact that you mentioned ‘bamboo spine’ and didn’t say ‘you’re gonna turn into a tree’ is honestly the most empathetic thing i’ve read all week 😭 i’ve been diagnosed for 6 years. i cry in the shower every morning. but i do my stretches. i swim. i take my pills. i don’t always feel like a person. but i’m still here. and this post? it didn’t sugarcoat it. thank you.
Gregory Clayton
bro. i went from ‘i can’t get out of bed’ to ‘i did a 5k’ in 18 months. no magic. just swim, stretch, and stop listening to people who say ‘rest is healing.’ rest is the enemy. movement is the drug. i don’t care if you’re 20 or 60. if you’re not moving, you’re dying slower. get up. go. now.
Catherine Scutt
why do people act like biologics are some kind of miracle? my cousin’s on Humira. Got a fungal infection so bad she lost two toes. Now she’s on antibiotics 24/7. The trade-off isn’t worth it if you’re just trying to ‘feel better.’ Maybe you should’ve started stretching before you got to this point. Now you’re just trading pain for infection.