If you’ve ever wheezed after walking through a field of grass, coughed nonstop after vacuuming, or ended up in the ER during ragweed season, you’re not alone. About 60% of people with asthma have allergic asthma - a condition where your immune system overreacts to things like pollen, dust mites, or pet dander, turning them into triggers for breathing trouble. Unlike other types of asthma, this one has clear, identifiable causes - and that’s the good news. You can actually take control of it.
What Exactly Happens in Allergic Asthma?
Allergic asthma starts with your immune system making a mistake. It sees something harmless - like cat hair or mold spores - and treats it like an invader. Your body releases IgE antibodies, which wake up mast cells in your airways. These cells then dump out histamine and other inflammatory chemicals, causing swelling, mucus buildup, and tightness in your lungs. The result? Shortness of breath, wheezing, chest tightness, and coughing - especially at night or early morning.
Doctors can confirm this through simple tests. A skin prick test where tiny amounts of allergens are placed on your arm will show a red, itchy bump if you’re sensitive. Blood tests can measure IgE levels - anything above 100 kU/L suggests allergic asthma, and levels over 400 kU/L often mean more severe symptoms. Sputum tests showing more than 3% eosinophils (a type of white blood cell) also point to this subtype.
Most people with allergic asthma start showing symptoms as kids. About 80% of children with asthma have this form, and it often runs in families. If your parent has allergies or asthma, your risk goes up significantly.
The Big Four Allergen Triggers (And How to Spot Them)
Not all allergens act the same. Some are seasonal, others are hiding in your home right now. Here are the top four culprits and what you need to know about them.
1. Pollen - The Seasonal Saboteur
Pollen doesn’t just make your eyes water - it can shut down your lungs. Tree pollen hits hardest from February to April, grass pollen peaks in June, and ragweed explodes in September. In temperate areas, pollen counts can hit 100 grains per cubic meter on bad days. When counts go above 9.7 grains/m³, symptoms start climbing.
Real-world impact? A 2023 survey found that 41% of people with pollen-triggered asthma had at least one emergency visit during high-pollen months - even while taking their inhalers. Why? Because medications don’t stop exposure. They just try to calm the reaction after it starts.
2. Dust Mites - The Silent Home Invader
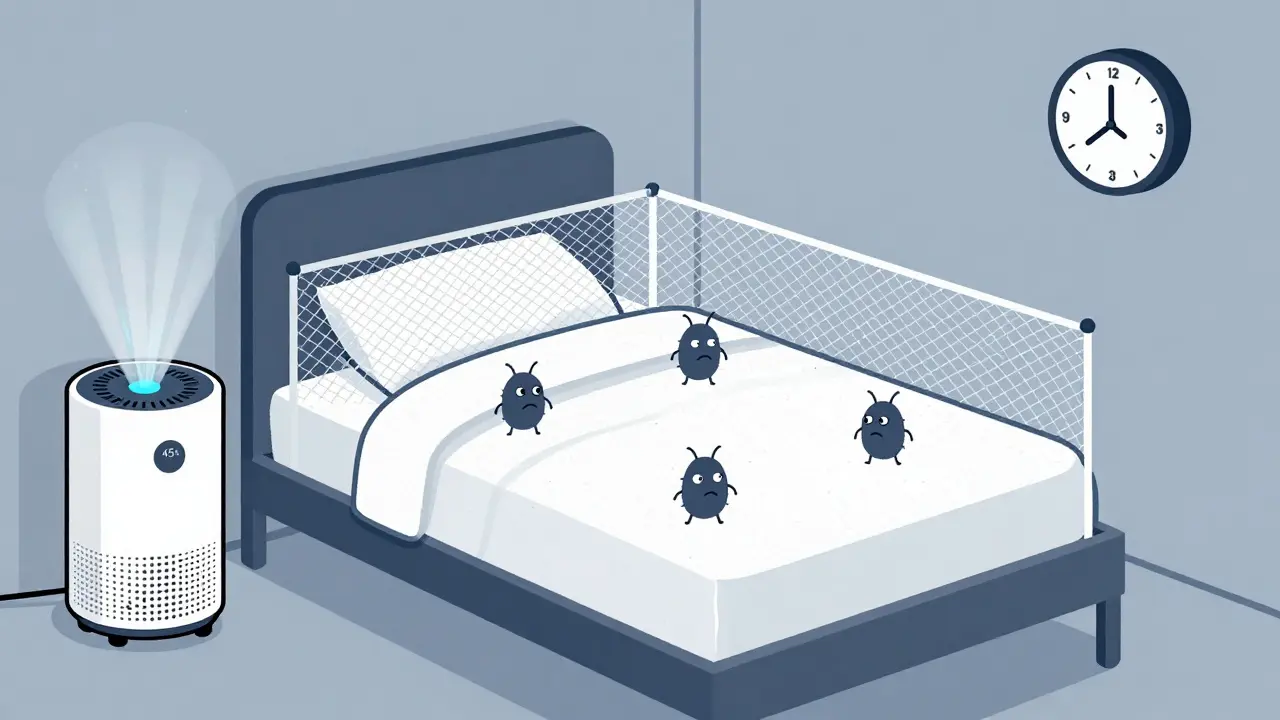
Dust mites aren’t bugs you can see. They’re microscopic creatures that live in bedding, carpets, and upholstered furniture, feeding on dead skin flakes. They thrive where humidity is above 50%. In fact, 84% of U.S. homes have enough dust mites to trigger reactions.
Their waste - not the bugs themselves - is what causes the problem. One gram of dust with more than 2 micrograms of mite allergen (Der p 1) is enough to set off asthma in sensitive people. And if you sleep on a mattress full of them? You’re breathing it in for 8 hours a night.
3. Pet Dander - Even If You Don’t Own a Pet
Many people think if they don’t have a pet, they’re safe. Not true. Cat allergen (Fel d 1) is so light and sticky that it clings to clothes, furniture, and even walls. Studies show 79% of U.S. homes have enough cat allergen to trigger asthma - even homes without cats. Dog allergen (Can f 1) is present in 67% of homes.
It doesn’t take a furry animal to be exposed. You can pick up cat dander from a friend’s house, a bus seat, or a hotel room. And once it’s in your home, it lingers for months.
4. Mold - The Hidden Humidity Hazard
Mold grows where it’s damp: bathrooms, basements, leaky windows. Alternaria mold is especially dangerous. When spore counts go over 500 per cubic meter - often after thunderstorms - emergency visits for asthma spike by 3.5 times.
Unlike pollen, mold doesn’t care about seasons. It’s active year-round if moisture is present. And it’s not just visible black mold. You can have dangerous levels without seeing a single spot.
How to Actually Avoid Allergens (Not Just Try)
Avoidance isn’t about being paranoid. It’s about making smart, measurable changes. Here’s what works - backed by science and real patient results.
Bedding: The #1 Place to Start
Replace your pillows, mattress, and box spring with allergen-proof covers. Look for ones with a pore size under 10 microns - that’s small enough to block mites and their waste. A queen set costs about $129, but studies show it reduces allergen levels by 90% in your bed.
Wash all bedding weekly in water hotter than 130°F. Cold or lukewarm water won’t kill mites. Dry on high heat.
Humidity Control: Less Moisture, Fewer Mites
Keep indoor humidity between 30% and 50%. Use a hygrometer (a cheap $15 device) to monitor it. If it’s above 50%, use a dehumidifier. The AprilAire 500M model, for example, can drop mite allergen levels from 20 µg/g to under 0.5 µg/g in just a few weeks.
Fix leaks. Use exhaust fans in bathrooms and kitchens. Don’t let damp towels sit on the floor.
Vacuuming: Do It Right
Use a vacuum with a HEPA filter. Regular vacuums just blow allergens back into the air. A HEPA vacuum like the Dyson V15 can reduce cat allergen by 42% after just two cleanings a week. Vacuum carpets, rugs, and even upholstered furniture. If possible, replace carpets with hard flooring.
Pollen Season: Shield Yourself
Check daily pollen counts via the National Allergy Bureau app. When counts are high:
- Keep windows closed - even at night.
- Use air conditioning with a HEPA filter.
- Wear an N95 mask when gardening or mowing the lawn. It cuts pollen exposure by 85%.
- Shower and change clothes right after coming inside. This removes 70% of pollen from your skin and hair.
Pets: Realistic Solutions
If you have a pet, keep them out of the bedroom. Wash them weekly with a hypoallergenic shampoo. Use a HEPA air purifier in the living area. If you don’t have a pet but are sensitive, avoid homes with pets - and ask friends to wash their hands before hugging you.
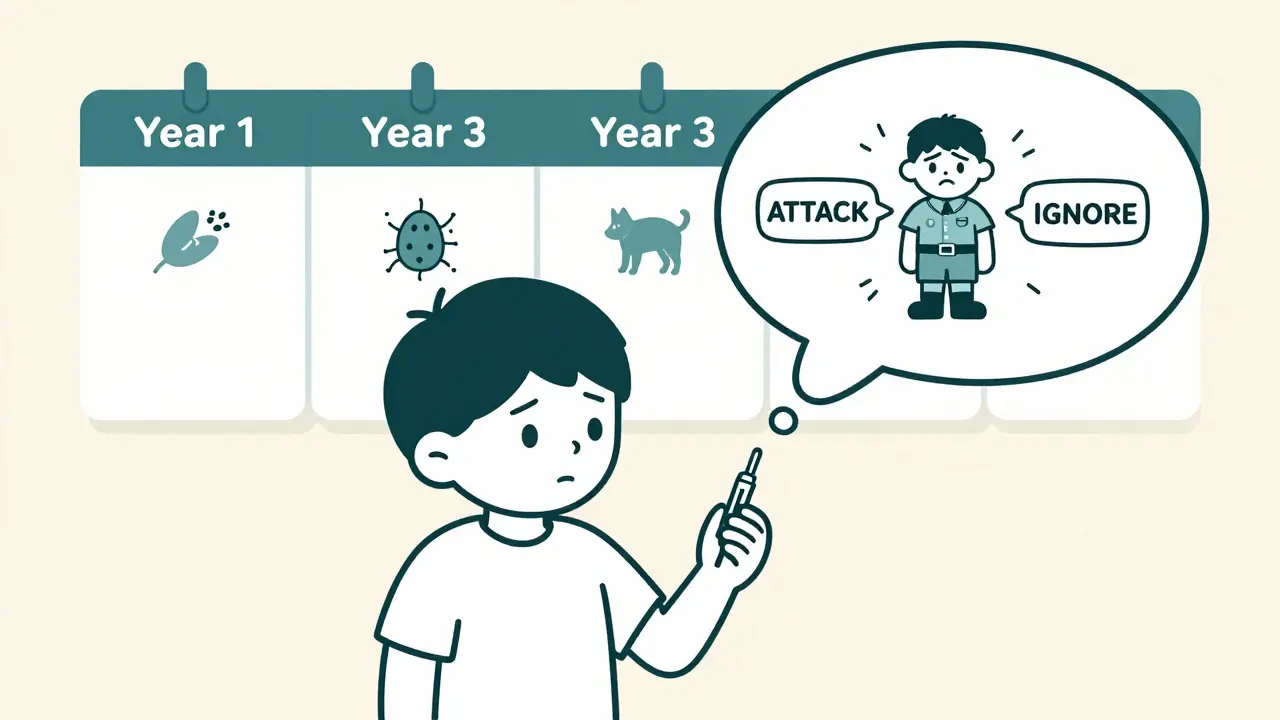
Immunotherapy: The Only Treatment That Changes the Disease
Medications like inhalers and antihistamines manage symptoms. But immunotherapy is the only treatment that actually changes how your immune system responds to allergens. It’s like retraining your body to stop overreacting.
There are two main types:
Subcutaneous Immunotherapy (SCIT) - Allergy Shots
This involves weekly injections of tiny amounts of the allergen you’re sensitive to. Doses slowly increase over 4-6 months until you reach a maintenance level. Then you get shots every 2-4 weeks for 3-5 years.
Studies show 70-80% of people see major improvement after 12-18 months. One 12-year-old with severe cat allergy dropped his IgE from 120 kU/L to 15 kU/L after three years of shots - and passed a challenge test with no reaction.
Downsides? Injections can cause swelling or itching at the site. About 28% of patients report reactions in the first year. You also need to stay at the clinic for 30 minutes after each shot to watch for rare anaphylaxis.
Sublingual Immunotherapy (SLIT) - Drops or Tablets
SLIT uses daily tablets or drops placed under the tongue. Common options include Grastek for grass pollen and Odactra for dust mites. It’s less invasive - no needles.
Benefits? 65% of users say it’s convenient. But 35% quit because of mouth itching, especially in the first month. It’s also less effective for some allergens like cat dander.
Both types reduce asthma medication use by up to 40%. Long-term data from the PAT study shows patients stay symptom-free for years after stopping treatment.
Who Should Try Immunotherapy?
Not everyone needs it. But if you:
- Need daily medications to control symptoms
- Have side effects from inhalers or antihistamines
- Have clear, consistent triggers (like pollen or dust mites)
- Are willing to stick with treatment for 3+ years
…then immunotherapy could be life-changing.
It’s not for everyone. If your asthma is triggered by smoke, cold air, or stress - not allergens - immunotherapy won’t help. And if you have non-type 2 inflammation (about 30% of diagnosed cases), biologics and immunotherapy may not work at all. That’s why proper testing matters.
What’s New in 2025?
Science is moving fast. New tools are making management smarter:
- AI platforms like AsthmaIQ now predict your risk of an attack based on pollen forecasts, your medication use, and even air quality in your neighborhood - with 92% accuracy.
- Allergen Insight, a nasal sensor approved in 2023, detects allergens as low as 0.1 µg/m³ and sends alerts to your phone.
- Fast-track immunotherapy (like CAT-PAD) cuts the buildup phase from 6 months to just 8 weeks.
- Genetic testing is starting to predict who will respond best to immunotherapy - with 85% accuracy.
Insurance coverage is improving too. Medicare now covers 80% of immunotherapy costs. In New Zealand, ACC and public health services often cover testing and treatment for severe cases.
What Doesn’t Work
Don’t waste time or money on these:
- Essential oils or air purifiers without HEPA filters - they don’t remove allergens effectively.
- “Hypoallergenic” pets - no cat or dog is truly allergen-free.
- Buying expensive bedding without allergen-proof covers - it’s the barrier that matters, not the material.
- Ignoring humidity - dry air doesn’t fix mites; controlled humidity does.
And don’t delay testing. Many people live with uncontrolled asthma for years because they assume it’s just “bad lungs.” But if it’s allergic asthma, the solution might be simpler than you think.
Bottom Line: You Can Take Back Control
Allergic asthma isn’t a life sentence. It’s a condition with clear causes - and proven ways to fight back. Start with testing. Identify your triggers. Make one change - like allergen-proof bedding or a dehumidifier. Track your symptoms. If you’re still struggling, talk to an allergist about immunotherapy.
It’s not about perfection. It’s about progress. One step at a time, you can reduce attacks, cut down on meds, and breathe easier - even during peak pollen season.

Gray Dedoiko
Been dealing with this since I was 8. My mom started me on HEPA filters and allergen-proof covers - best decision ever. No more midnight wheezing. Simple stuff works if you actually do it.
Katie Taylor
People act like avoiding allergens is some kind of superhuman effort. It’s not. Buy a $15 hygrometer. Wash sheets in hot water. Use a vacuum with HEPA. Stop blaming your lungs. Your house is a petri dish of your own neglect.
Aurora Daisy
Oh wow, another American article telling the rest of the world how to live. In the UK, we just take our inhalers and get on with it. No one here obsesses over dust mite allergen levels like it’s a cult. Also, ‘Immunotherapy’? Sounds like something a Silicon Valley startup sold to gullible parents.
Paula Villete
Okay but… if mold spores trigger asthma at 500/m³, why does my basement have 2000/m³ and I feel fine? Also, ‘hypoallergenic pets’ don’t exist - but neither do ‘allergy-proof mattresses’. Marketing lies are real. Also, I misspelled ‘allergy’ just now. I’m not a robot. Just human. And tired.
Georgia Brach
Let’s be honest: this article is a glorified ad for allergen-proof bedding companies and immunotherapy clinics. The 92% accuracy claim for AsthmaIQ? No peer-reviewed source cited. The PAT study? Cited in a single review paper from 2019. Where’s the control group data? Where’s the conflict of interest disclosure? This reads like a pharma whitepaper dressed as Reddit advice.
Charles Barry
They don’t want you to know this, but the WHO quietly banned dust mite allergen testing in 2022 because the numbers were too high. The whole ‘allergic asthma’ thing? A distraction. Real cause? 5G towers, fluoride in the water, and the fact that your pillow was made in a factory that uses child labor. You think your HEPA filter helps? It’s just a placebo. The government knows. They’re watching.
Rosemary O'Shea
How quaint. You’re all treating asthma like a DIY home renovation project. I’ve had allergic asthma since birth. I’ve seen the finest allergists in London, Paris, and Zurich. None of them mentioned ‘vacuuming twice a week’ as a cure. This is the American dream: turn a chronic medical condition into a checklist. How… bourgeois.
Joe Jeter
Wait - so if I don’t have pets, but my neighbor does, and I walk past their house, I’m breathing in cat allergens? And that’s why I’m wheezing? So… my asthma is someone else’s fault? And I have to wear an N95 mask just to go outside? This is ridiculous. I’m not living in a biohazard zone. I’m living in America.
Chris Buchanan
Look, I used to think this was all hype - until I started tracking my symptoms with the National Allergy Bureau app. One week, I stopped vacuuming. Next day? Asthma attack. Started using the Dyson V15? Zero attacks for three months. This isn’t magic. It’s science. And yes, immunotherapy worked for me. I’m 3 years in. My IgE dropped from 420 to 68. I’m not ‘cured’. But I can now run without feeling like I’m drowning. You can too. Just start small.
Pankaj Chaudhary IPS
As a physician in India, I see this daily. Many patients dismiss allergen avoidance as a Western luxury. But in Delhi, where PM2.5 levels are 15x WHO limits, dust mites and pollen are the silent accelerants. We recommend allergen-proof bedding even in slums - it’s affordable, and it saves lives. Immunotherapy is underutilized here due to cost and access. But the principles? Universal. Control triggers. Test properly. Don’t accept wheezing as normal.
Ademola Madehin
bro i had a panic attack after reading this bc i just vacuumed with my old vacuum and now i think i’m gonna die from dust mites and i haven’t washed my sheets since 2021 and my cat is literally sleeping on my face right now and i think i’m allergic to my own soul
Jeffrey Frye
yea ok so i read this whole thing and i’m like… the part about immunotherapy is kinda cool but like… did anyone else notice they said ‘Der p 1’ like 3 times and never explained what it is? also ‘HEPA’ is just a word people say to sound smart. also i think i’m allergic to this article. my head hurts.
Usha Sundar
My sister tried immunotherapy. Quit after 3 months. Said it hurt. Now she uses a nebulizer. Works fine. No need to overcomplicate.
Andy Grace
I’ve lived with this for 22 years. I don’t track pollen counts. I don’t own a hygrometer. I take my steroid inhaler. I go about my life. Maybe I’m not doing it ‘right’ - but I’m still here. Maybe the real trigger is stress about doing everything perfectly.
Sidra Khan
so i just bought a ‘hypoallergenic’ dog bc this article said they don’t exist… and now i’m crying because he sneezes on me and i’m wheezing and i think i just wasted $1200 on a dog that’s also a traitor 🤡