Don’t Guess When You Grab That Bottle
Every day, millions of people pick up OTC medications without a second thought. A headache? Grab Tylenol. A stuffy nose? Reach for the cold tablet. But here’s the truth: OTC medications aren’t harmless. They’re powerful chemicals, and using them wrong can land you in the ER. In 2022, over 198,000 single-substance OTC medication exposures were reported to U.S. poison control centers. Most of these weren’t accidents-they were mistakes. Misunderstood labels. Overlapping ingredients. Wrong doses. You don’t need to be a pharmacist to use OTC meds safely. You just need to know what to look for.
Read the Drug Facts Label-Every Time
The FDA made this easy. Since 1999, every OTC medicine sold in the U.S. must have a standardized Drug Facts label. It’s not a suggestion. It’s the law. And it’s your best friend. Don’t just glance at the brand name. Don’t skip to the directions. Read the whole thing. It’s designed to be clear: active ingredients, purpose, uses, warnings, directions, other information. The label changes. A product you used last year might have a new warning or a different dose. That’s why you read it every time-even if it’s the same bottle you’ve used for years.
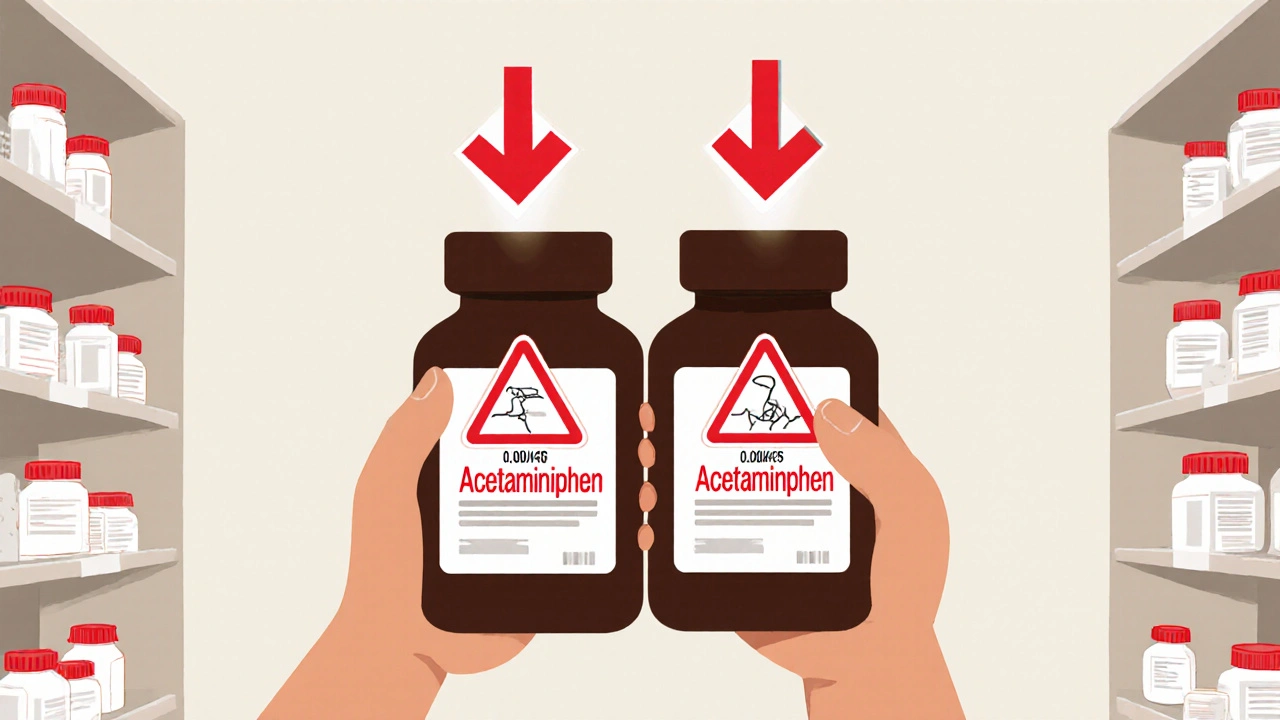
Know Your Active Ingredients
Here’s where most people get hurt. You take a cold tablet. Then you take a pain reliever. Then you take a sleep aid. All seem fine. But if they all contain acetaminophen, you’re overloading your liver. Acetaminophen is in over 600 OTC products-from Tylenol to NyQuil to Excedrin. The FDA says more than 56,000 emergency room visits each year are caused by too much acetaminophen. It doesn’t take much. Just 10 grams in one day can cause serious liver damage. The same goes for ibuprofen, naproxen, and antihistamines. Always check the active ingredient list. If two products have the same one, don’t take them together. Your body doesn’t care what brand it’s in. It only cares about the chemical.
Use Only What You Need
Multi-symptom cold remedies are a trap. They promise relief from cough, congestion, fever, and sore throat-all in one pill. But if you only have a runny nose, why are you taking something that also makes you drowsy and raises your blood pressure? The Ohio Department of Aging says it best: pick medications that treat only the symptoms you have. That means avoiding products with ingredients you don’t need. A decongestant like pseudoephedrine can spike your blood pressure. Antihistamines like diphenhydramine can cause dizziness and confusion, especially in older adults. If you’re diabetic, pregnant, or have heart disease, some of these ingredients can be dangerous. Talk to your pharmacist before taking anything that claims to fix five things at once.
Dosage Isn’t Guesswork
Children aren’t small adults. And neither are you, if you’re over 65. The FDA is clear: never estimate a dose based on weight or size. Use the measuring tool that comes with the medicine. A tablespoon is not a teaspoon. A kitchen spoon varies by up to 200% in volume. One study found that nearly half of people used household spoons to measure liquid medicine. That’s how overdoses happen. For adults, stick to the label. For kids, use the dosing cup or syringe. If you’re unsure, ask the pharmacist to show you how to measure it. It’s free. And it’s worth it.

Pharmacists Are Your Secret Weapon
Most people think pharmacists just hand out pills. They’re wrong. Pharmacists are trained to spot dangerous combinations, hidden risks, and outdated advice. A 2022 study showed pharmacist consultations reduced OTC medication errors by 67%. They know which antihistamine is safer for someone with an enlarged prostate. They know which pain reliever won’t clash with your blood thinner. They know why you shouldn’t mix alcohol with dextromethorphan. And they do it for free. Walk up to the counter. Say: “I’m thinking of buying this for my headache and cold. I also take [list your prescriptions]. Is this safe?” Don’t be shy. Pharmacists want you to ask. They’re there to keep you safe.
Know Your Health Conditions
Some OTC meds are fine for most people-but dangerous for you. If you have diabetes, avoid decongestants-they can raise blood sugar. If you have high blood pressure, avoid NSAIDs like ibuprofen for long periods-they can spike your pressure. If you have kidney disease, avoid NSAIDs entirely. If you’re pregnant or breastfeeding, skip certain antihistamines and pain relievers. The Merck Manual says older adults make up half of all adverse drug reactions, even though they’re only 13% of the population. Why? Because their bodies process drugs slower. And they’re often on multiple medications. If you’re taking more than five prescriptions or OTCs, you’re at higher risk. Always tell your pharmacist everything you take-supplements included.
Check for Interactions
OTC meds don’t just interact with other drugs. They interact with alcohol, caffeine, even food. Mixing alcohol with antihistamines can cause extreme drowsiness. Mixing alcohol with acetaminophen increases liver damage risk. Sleep aids like doxylamine shouldn’t be taken with prescription sedatives. Aspirin can thin your blood-so if you’re on warfarin, don’t take it without checking. The FDA warns: if you’re unsure, talk to a professional. Don’t Google it. Don’t ask a friend. Don’t assume it’s safe because it’s “just OTC.”
Use the Same Pharmacy
It sounds simple, but it matters. If you buy your OTC meds at different stores, no one has a full picture of what you’re taking. Your pharmacist can’t warn you about interactions if they don’t know you bought a cold medicine last week at another pharmacy. Using the same pharmacy means your medication history is tracked. They can flag potential problems before you even walk up to the counter. It’s not about loyalty. It’s about safety.

When to Skip OTC and See a Doctor
OTC meds are for minor, short-term issues. If your symptoms last more than a week, get worse, or come with a fever, rash, or confusion, stop taking it and see a doctor. Don’t keep doubling up. Don’t “wait and see.” That’s how small problems turn into big ones. If you’re over 65, pregnant, or have a chronic illness, don’t self-treat for more than a few days. Your body isn’t the same as it was ten years ago. What worked then might not be safe now.
What’s Changing in 2025?
The FDA is updating its OTC drug review system for the first time in decades. The CARES Act of 2020 started this process, and by 2025, new labeling rules and faster updates to safety info will be in place. That means more accurate warnings, clearer directions, and better alerts for interactions. But until then, you still need to be the one reading the label. Don’t wait for the system to fix itself. Be the person who reads it. Who asks questions. Who checks ingredients. That’s how you stay safe.
Quick Summary
- Always read the Drug Facts label-every single time.
- Know the active ingredients. Never combine products with the same one.
- Use only what you need. Avoid multi-symptom products unless necessary.
- Measure doses accurately. Never use kitchen spoons.
- Talk to your pharmacist. It’s free and saves lives.
- Don’t take OTC meds if you have certain health conditions without checking first.
- Use the same pharmacy so your medication history is tracked.
- If symptoms last more than a week or get worse, see a doctor.
Can I take two different OTC pain relievers at the same time?
Only if they don’t share the same active ingredient. For example, you can take ibuprofen and acetaminophen together because they work differently. But never take two products that both contain acetaminophen-like Tylenol and a cold medicine. That’s how you overdose. Always check the active ingredient list on the label.
Is it safe to use OTC meds if I’m pregnant?
Some are, some aren’t. Acetaminophen is generally considered safe for occasional use during pregnancy, but avoid ibuprofen and naproxen, especially in the third trimester. Decongestants like pseudoephedrine can reduce blood flow to the placenta. Antihistamines like diphenhydramine may cause drowsiness in the baby. Always talk to your doctor or pharmacist before taking anything-even if it’s labeled "OTC."
Why do some OTC medicines say "do not use if you have high blood pressure"?
Because ingredients like pseudoephedrine and phenylephrine are decongestants that narrow blood vessels. That’s how they reduce nasal swelling-but they also raise your blood pressure. If you already have high blood pressure, these can push it into dangerous territory. Even if your pressure is controlled, these meds can interfere with your medication. Always check the warning section.
Are natural or herbal OTC remedies safer?
Not necessarily. Many herbal products aren’t regulated the same way as FDA-approved OTC drugs. You won’t find a Drug Facts label. Dosing is unclear. Interactions are poorly studied. St. John’s Wort, for example, can make birth control, antidepressants, and blood thinners less effective. Just because something is "natural" doesn’t mean it’s safe. Always treat herbal remedies like medicine-ask your pharmacist before using them.
How do I know if I’m taking too much acetaminophen?
The maximum daily dose for adults is 4,000 milligrams. But many people exceed that without realizing it. If you take Tylenol, then a cold medicine with acetaminophen, then a sleep aid with it, you’ve likely gone over. Signs of overdose include nausea, vomiting, loss of appetite, and pain in the upper right side of your abdomen. But here’s the scary part: you might feel fine for days. Liver damage can be silent until it’s too late. Always count your acetaminophen intake from all sources.
Should I keep a list of my OTC medications?
Yes. Write down what you take, how often, and why. Include the brand and active ingredient. Bring it to every doctor’s visit-even if you think it’s not important. Pharmacists and doctors need to see the full picture. Many adverse reactions happen because no one knew you were taking a cold medicine with ibuprofen while on a blood thinner. A simple list can prevent a hospital visit.
Final Thought
OTC medications are tools, not toys. They help when used right. They hurt when used wrong. The difference isn’t in the bottle. It’s in the person holding it. Read the label. Know your ingredients. Ask the pharmacist. Don’t guess. You’ve got this.
fiona collins
Always read the label. Every. Single. Time. I used to skip it-until I ended up with liver enzymes through the roof. Don't be me.
giselle kate
This is why America’s healthcare system is broken-people won’t take responsibility. You want safety? Stop relying on pharmacists. Learn. Yourself. The label isn’t rocket science. It’s English. Read it.
Karen Willie
I love how this post reminds us that we don’t need to be experts to stay safe. Just curious. And willing to ask. That’s enough. 🌱
Leisha Haynes
Multi-symptom meds are the scam of the century 🙄 I used to buy them like candy until I realized I was taking 3 different antihistamines and wondering why I felt like a zombie. Duh.
Shivam Goel
Let’s be real-acetaminophen overdose is a public health failure. 56,000 ER visits annually? That’s not ignorance-it’s systemic. Pharma marketing pushes combo products. Regulators lag. Consumers get poisoned. The FDA’s 2025 update? Too little. Too late. We need mandatory dose caps on OTC bottles. And mandatory pharmacist consultation for anyone over 50. Not optional. Mandatory.
Andrew McAfee
In India, we don’t have Drug Facts labels. We have shopkeepers handing out pills with no idea what’s in them. This post? It’s a blueprint. Maybe we need to export this model. Not just the meds-the mindset.
Roscoe Howard
It is imperative to note that the utilization of over-the-counter pharmaceutical agents without comprehensive knowledge of their pharmacokinetic profiles constitutes a significant public health liability. The absence of physician oversight in this domain is not merely inadvisable-it is statistically correlated with increased morbidity and mortality rates, particularly among geriatric populations.
Kimberley Chronicle
The pharmacovigilance angle here is critical-polypharmacy risk stratification is underutilized in OTC contexts. Leveraging pharmacy-based medication reconciliation protocols can reduce adverse drug events by up to 67%, per the 2022 JAMA study cited. We need embedded clinical decision support at the point of sale.
Shirou Spade
We treat medicine like candy because we’ve forgotten that everything is a poison-the dose just makes it a remedy. The real question isn’t how to read the label-it’s why we ever stopped trusting our own bodies to tell us what we need. We’ve outsourced healing to corporations and expect them to be our conscience.
Lisa Odence
This is the most important post I’ve read all year 🙏 I literally printed this out and taped it to my medicine cabinet. Also, I started using the same pharmacy last month and my pharmacist remembered I take warfarin and stopped me from buying a cold med with pseudoephedrine 😭 Thank you for writing this. I’m telling everyone. 💯❤️