Why Your Kidneys Need a Special Diet
When your kidneys aren’t working right, they can’t filter out the extra salt, potassium, and phosphorus from your food. That stuff builds up in your blood and can cause serious problems-high blood pressure, heart rhythm issues, weak bones, or even a heart attack. A renal diet isn’t about eating less-it’s about eating smarter. It’s the difference between keeping your kidneys working longer and needing dialysis sooner.
Sodium: The Silent Blood Pressure Killer
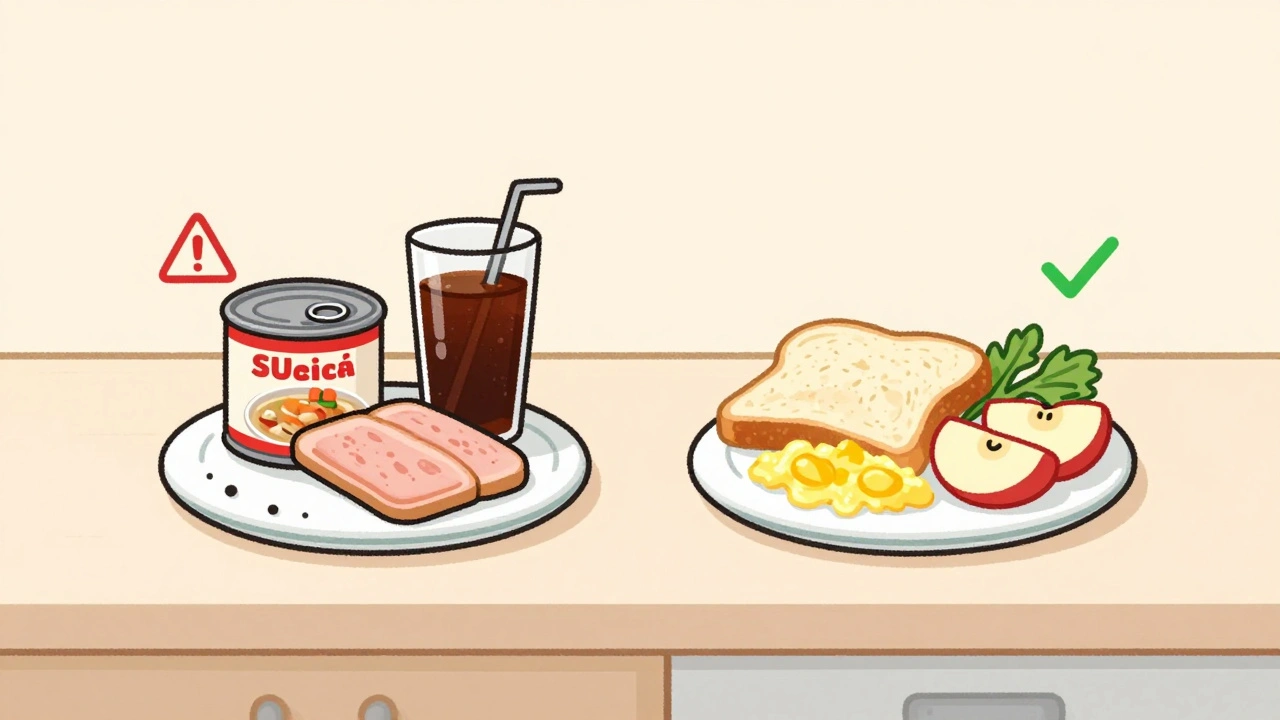
Most people don’t realize how much sodium is hiding in their food. About 75% of it comes from packaged and processed items, not the salt shaker. A single can of soup can have more sodium than you’re supposed to eat in a whole day. For someone with kidney disease, the goal is to stay under 2,000-2,300 milligrams per day. That’s less than one teaspoon of table salt.
Reading labels is non-negotiable. Look for "low sodium," "no salt added," or "unsalted." Avoid anything with sodium benzoate, sodium nitrate, or monosodium glutamate (MSG). Canned vegetables, frozen meals, deli meats, and soy sauce are all sodium traps. Instead, flavor food with herbs like basil, oregano, or garlic powder. Mrs. Dash and similar blends work well because they add taste without sodium.
Lowering sodium doesn’t just help your kidneys-it helps your heart. Cutting 1,000 mg of sodium a day can drop your systolic blood pressure by 5 to 6 points. That’s the same effect as some blood pressure meds, without the side effects.
Potassium: The Fine Line Between Safe and Dangerous
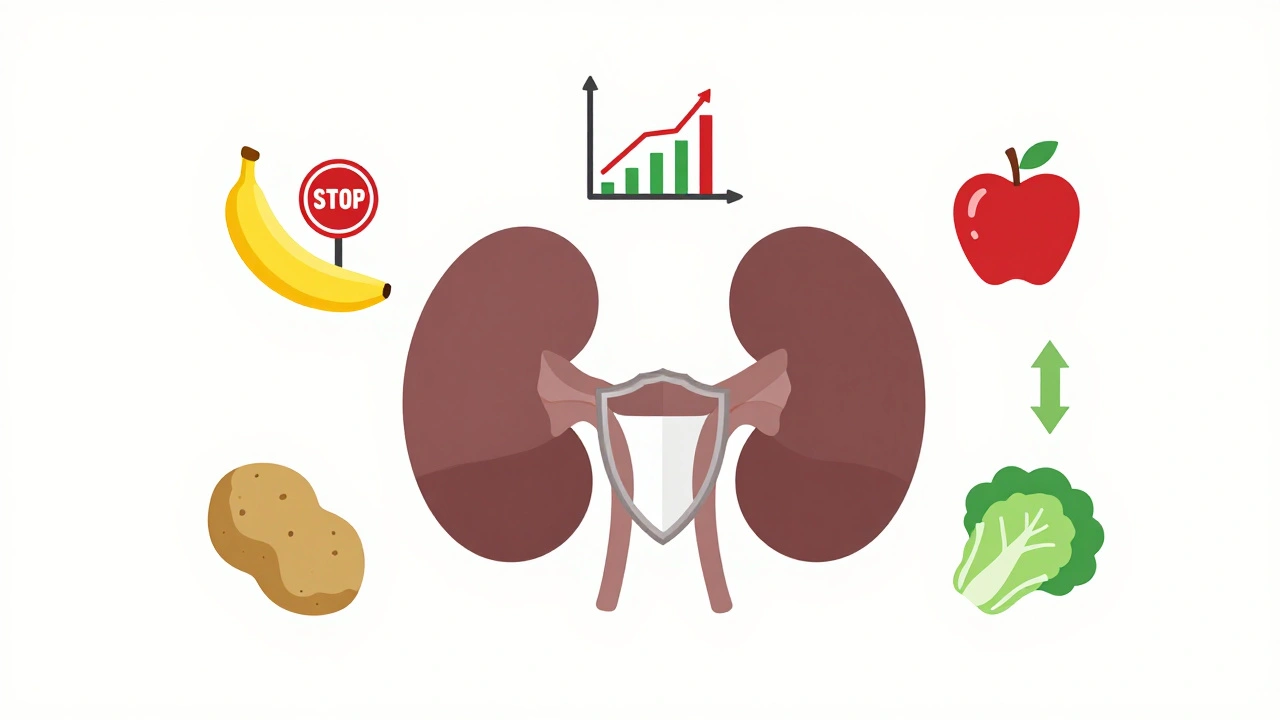
Potassium keeps your heart beating regularly. But when your kidneys can’t remove it, levels climb. Above 5.5 mEq/L, it can trigger dangerous heart rhythms. That’s why most people with stage 3-5 kidney disease need to keep potassium under 2,000-3,000 mg per day.
Not all fruits and veggies are safe. Bananas, oranges, potatoes, tomatoes, and spinach are packed with potassium. One medium banana has 422 mg. A cup of cooked spinach? Over 800 mg. That’s more than half your daily limit in one serving.
But you don’t have to give up produce entirely. Apples, berries, cabbage, green beans, and cauliflower are low-potassium options. A medium apple has just 150 mg. Half a cup of blueberries? Only 65 mg. Leaching vegetables can help too-soak sliced potatoes or carrots in warm water for 2-4 hours, then boil them in plenty of water. That cuts potassium by about half.
Here’s the twist: potassium from animal foods (like meat and dairy) is absorbed more easily than from plants. So even if you eat a plant-based diet, you still need to watch portions. A 3-ounce serving of salmon is fine, but four ounces might push you over your limit.
Phosphorus: The Hidden Threat in Processed Foods
Phosphorus is tricky because not all of it comes from natural sources. Your body absorbs only about 50-70% of phosphorus from whole foods like chicken, beans, or dairy. But when it’s added as a preservative or flavor enhancer-like in colas, processed cheese, or frozen pizzas-your body absorbs 90-100% of it.
That’s why dietitians tell you to avoid anything with "phos" in the ingredient list: phosphoric acid, sodium phosphate, calcium phosphate. A 12-ounce cola has 450 mg. One slice of processed cheese? 250 mg. That’s nearly half your daily limit in one snack.
Stick to fresh meats, eggs, and unprocessed dairy. A half-cup of milk has 125 mg. White bread has 60 mg per slice. Whole-grain bread? 150 mg. So swap whole grain for white bread if you need to cut phosphorus. Rice and pasta made from refined grains are better choices than brown rice or whole-wheat versions.
Some newer foods are designed for kidney patients. In 2023, the FDA approved Keto-1, a medical food that provides protein without the phosphorus load. And research shows certain prebiotic fibers, like inulin, may reduce phosphorus absorption by 15-20%.

What You Can Eat: Real Meal Examples
Here’s what a day on a renal diet might look like:
- Breakfast: White toast (2 slices), scrambled egg, apple slices, unsweetened tea
- Lunch: Grilled chicken breast (3 oz), white rice, steamed green beans, pear
- Dinner: Baked cod (3 oz), mashed potatoes (leached), sautéed cabbage, cranberry juice
- Snacks: Rice cakes, low-potassium fruit like grapes or pineapple, unsalted popcorn
Portion control matters more than you think. A small serving of a high-potassium food is safer than a large serving of a low-potassium one. A half-cup of cooked broccoli is okay. A whole cup? Probably not.
Fluids, Protein, and Other Rules
Fluid intake isn’t always part of the renal diet-but it often is. If you’re producing less than a liter of urine a day, you’ll likely need to limit fluids to 32 ounces (about 1 liter). That includes water, coffee, soup, ice cream, and even gelatin. Sucking on ice chips or lemon slices can help with thirst without adding volume.
Protein is another balancing act. Too much stresses your kidneys. Too little leads to muscle loss and weakness. The current recommendation is 0.55 to 0.8 grams of high-quality protein per kilogram of body weight. That means a 150-pound person needs about 42-60 grams a day. Eggs, lean meat, fish, and poultry are best. Avoid plant proteins like beans and lentils-they’re high in phosphorus and potassium.
Why This Diet Works: The Science Behind It
Studies show that sticking to a renal diet can delay dialysis by 6 to 12 months in stage 4 kidney disease. That’s not just a number-it’s a year of independence, fewer hospital visits, and better quality of life.
Medicare now covers 3 to 6 sessions per year with a renal dietitian for stage 4 patients. Why? Because it saves money. Delaying dialysis saves about $12,000 per patient each year. The system is catching on: the global renal nutrition market is expected to hit $3.2 billion by 2030.
And it’s not one-size-fits-all anymore. The latest guidelines from KDIGO (2023) stress personalization. Your potassium limit might be 2,500 mg. Mine might be 2,000. It depends on your blood tests, urine output, and other health conditions. That’s why working with a renal dietitian is so important.
Common Mistakes and How to Avoid Them
- Assuming "healthy" means kidney-safe. Kale, avocado, sweet potatoes, and nuts are healthy-but they’re dangerous for kidneys. Swap them out.
- Using salt substitutes. Many contain potassium chloride. That’s worse than regular salt if your potassium is already high.
- Skipping meals. You need enough calories to prevent muscle wasting. Use oils, sugar, and white bread to add calories without phosphorus or potassium.
- Not tracking intake. Apps like Kidney Kitchen let you scan barcodes and track sodium, potassium, and phosphorus in real time. Download one. It helps.
What’s New in 2025
Technology is making this diet easier. Mayo Clinic is testing AI apps that sync with your lab results. If your potassium spikes, the app adjusts your meal plan automatically. The NIH’s PRIORITY study is looking at genetic markers that predict how your body handles potassium and phosphorus-personalized diet plans based on your DNA might be a reality soon.
Some experts are pushing back on strict limits. A 2023 review in JAMA Internal Medicine suggested that moderate restriction-with focus on food quality over extreme limits-may be better long-term. But that doesn’t mean you can go back to your old diet. It means you need to be smarter, not stricter.
Final Thoughts: This Isn’t a Diet. It’s a Lifeline.
A renal diet isn’t about deprivation. It’s about protecting your body so you can keep living well. You don’t have to give up flavor. You don’t have to eat bland food. You just need to know what’s safe and what’s not.
Start small. Pick one thing to change this week-maybe swap soda for sparkling water, or switch from whole-grain bread to white. Talk to your doctor or dietitian. Get your blood levels checked. Then adjust from there.
Your kidneys are working hard for you. Give them the support they need.
Can I still eat fruits and vegetables on a renal diet?
Yes, but you need to choose carefully. Low-potassium options like apples, berries, cabbage, green beans, and cauliflower are safe in controlled portions. Avoid high-potassium choices like bananas, oranges, potatoes, tomatoes, and spinach. Leaching vegetables by soaking and boiling them can reduce potassium by up to 50%.
Is it okay to use salt substitutes?
No. Most salt substitutes replace sodium chloride with potassium chloride. If your kidneys can’t clear potassium, this can raise your blood levels to dangerous levels-leading to heart rhythm problems. Stick to herb blends like Mrs. Dash or garlic powder instead.
Why are phosphorus additives worse than natural phosphorus?
Your body absorbs nearly all the phosphorus added to processed foods-up to 90-100%. Natural phosphorus in meat or dairy is only 50-70% absorbed. That’s why colas, processed cheese, and frozen meals are more harmful than a steak or a glass of milk. Always check labels for "phos" in the ingredients.
Do I need to limit protein on a renal diet?
Yes, but not drastically. Too much protein strains your kidneys. Too little causes muscle loss. The current guideline is 0.55-0.8 grams of high-quality protein per kilogram of body weight. That’s about 40-60 grams a day for most people. Focus on eggs, fish, and lean meat. Avoid beans, lentils, and soy products-they’re high in phosphorus and potassium.
Can I drink coffee or tea on a renal diet?
Yes, in moderation. One cup of black coffee has about 116 mg of potassium and 60 mg of phosphorus. If you’re on fluid restrictions, count it as part of your daily fluid limit. Avoid creamers and sweeteners that contain hidden sodium or phosphorus. Herbal teas without added minerals are usually safe.
How long does it take to adjust to a renal diet?
Most people need 3 to 6 months to get used to the changes. The first challenge is flavor-food can taste bland without salt. The second is planning meals. Using apps, keeping a food journal, and working with a dietitian helps. Over time, your taste buds adapt, and the diet becomes routine.
Are there foods specifically made for kidney patients?
Yes. In 2023, the FDA approved Keto-1, a medical food designed to provide essential amino acids while minimizing phosphorus and potassium. There are also low-phosphorus rice varieties and specialized kidney-friendly snacks available through medical suppliers. These aren’t necessary for everyone, but they help when standard foods are too high in minerals.
What if I have diabetes too?
It’s more challenging. Many heart-healthy foods for diabetics-like whole grains, beans, and fruit-are high in potassium and phosphorus. You’ll need to find a balance. Work with a dietitian who specializes in both diabetes and kidney disease. Focus on low-potassium fruits like apples and berries, and use white rice instead of brown. Portion control is even more critical.
Shannara Jenkins
Just started my renal diet last week and honestly? It’s way less scary than I thought. Swapped soda for sparkling water with a squeeze of lemon-game changer. I still eat fruits, just pick the low-potassium ones like apples and grapes. Mrs. Dash on everything. My taste buds are adjusting, and I feel better already. You got this.
Elizabeth Grace
I miss salt so bad I cry sometimes. Like, I literally sat in the grocery store aisle crying over a bag of pretzels. Then I remembered my creatinine was 4.8 last month. Now I just stare at them like they’re my ex. Still don’t eat them. But I dream about them. Every. Night.
Jay Everett
Yo, this guide is FIRE 🔥. Seriously, the part about phosphorus additives being 90-100% absorbed? Mind blown. I used to chow down on frozen pizzas like they were snacks. Now I read every label like it’s a spy novel. "Phosphoric acid"? BANNED. "Calcium phosphate"? GONE. I even switched to white bread because my kidneys said "nope" to whole grain. 🤖💡 And yes, Keto-1 exists-I tried it. Tastes like chalky protein pudding, but my phosphorus levels dropped 20%. Worth it. Also, leaching potatoes? Magic. Soak ‘em, boil ‘em, eat ‘em. Your kidneys will high-five you.
Rebecca M.
Oh great, another article telling me I can’t eat anything delicious. Next they’ll tell me to stop breathing. Because apparently, if I enjoy life, my kidneys will revolt. 🙄
Paul Keller
While the general principles outlined here are sound, one must critically evaluate the underlying assumptions. The assumption that sodium restriction universally improves outcomes is not without controversy. Recent meta-analyses, including those from the Cochrane Collaboration, suggest that the benefit of sodium restriction below 2,300 mg/day in chronic kidney disease is marginal at best, particularly in non-hypertensive populations. Moreover, the demonization of phosphorus additives ignores the fact that endogenous phosphorus regulation is a complex interplay of FGF-23, vitamin D, and parathyroid hormone-not merely a function of dietary intake. The recommendation to avoid whole grains while favoring refined carbohydrates is not only nutritionally regressive, but potentially pro-inflammatory. One must ask: are we optimizing for lab values, or for long-term metabolic health? The answer, as always, lies not in dogma, but in individualized, evidence-based physiology.
Alicia Marks
Low-potassium fruits = your new BFFs. Apples, berries, grapes. Done. You got this.
Roger Leiton
Wait, so if I eat a banana and then take a phosphate binder, does that cancel it out? 😅 I’m just asking for a friend… who is me. Also, has anyone tried the new kidney-friendly ice cream? I heard it’s made with rice milk and has zero phosphorus. I need hope.
Steve Enck
The entire paradigm of renal dietary management is predicated upon a reductionist model of nephrology that ignores systemic homeostatic feedback loops. The focus on macronutrient quantification-sodium, potassium, phosphorus-reduces the kidney to a mere filtration unit, neglecting its endocrine, metabolic, and immunomodulatory functions. Furthermore, the promotion of white bread over whole grain, under the guise of phosphorus reduction, perpetuates a iatrogenic cascade of insulin resistance and systemic inflammation, which are themselves independent risk factors for cardiovascular mortality in CKD. One must interrogate the source of these guidelines: are they derived from randomized controlled trials, or from the commercial interests of the medical food industry? The approval of Keto-1, while seemingly benevolent, represents a commodification of necessity. The true intervention is not dietary restriction, but early nephroprotection through RAAS blockade and glycemic control. This is not nutrition-it is symptom management dressed as prevention.
Lynn Steiner
USA rules. We don’t need fancy medical foods. Just eat real food. But since you’re on dialysis, you’re basically a walking lab rat anyway. 🇺🇸❤️