When it comes to keeping your blood Calcium in check, calcitonin is the hormone that often flies under the radar. While most people hear about parathyroid hormone (PTH) as the main regulator, calcitonin works as the “brake” that slows down calcium release from bone. This article breaks down how calcitonin fits into the larger calcium‑homeostasis system, why it matters for bone health, and what clinicians do with it in real‑world practice.
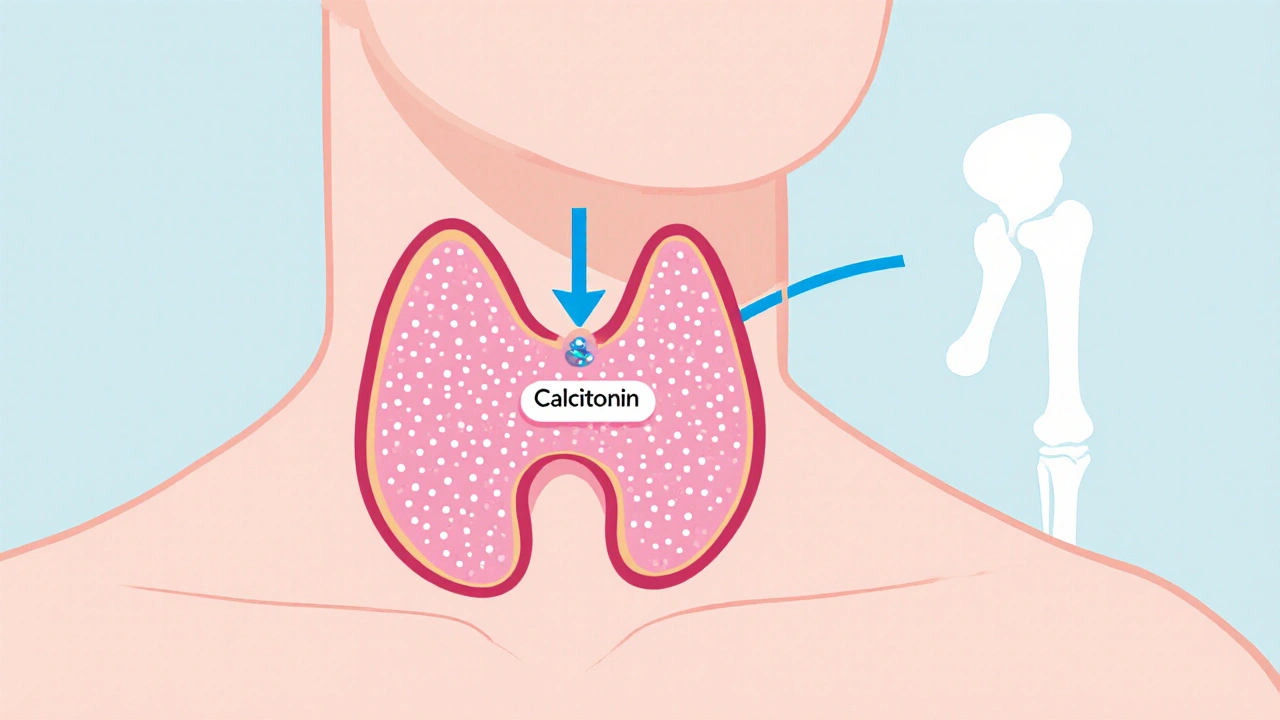
What Is Calcitonin?
Calcitonin is a peptide hormone produced by the thyroid gland, specifically the C‑cells (also called parafollicular cells). Its primary job is to lower blood calcium levels when they rise too high. It does this by instructing osteoclast cells - the bone‑resorbing cells - to slow their activity, which reduces the amount of calcium released from the bone matrix into circulation.
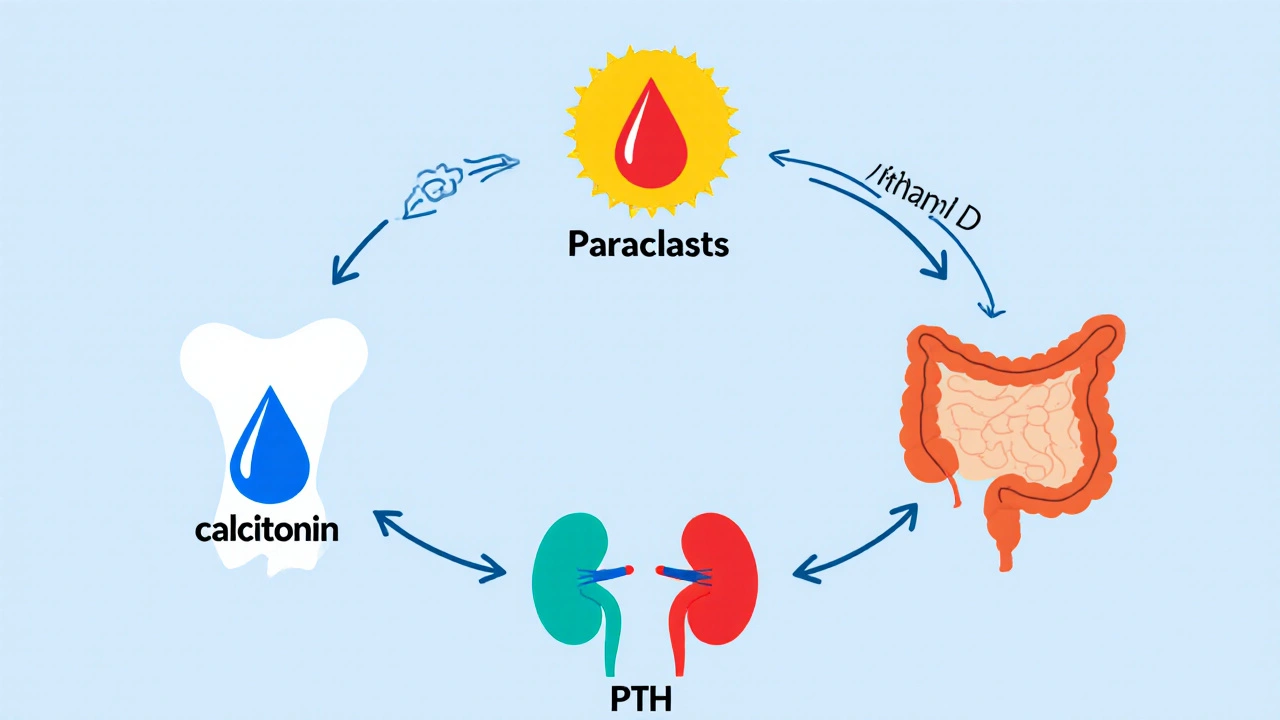
How Calcitonin Controls Calcium Homeostasis
Calcium homeostasis is a tightly regulated loop involving three main players: calcitonin, PTH, and Vitamin D. When blood calcium spikes after a calcium‑rich meal, the thyroid’s C‑cells secrete calcitonin. The hormone binds to receptors on osteoclasts, triggering a cascade that reduces bone resorption. In parallel, the kidneys increase calcium excretion, and the gut reduces calcium absorption. Together these actions bring serum calcium back toward the normal range (about 8.5‑10.5 mg/dL for adults).
Calcitonin vs. Parathyroid Hormone: A Quick Contrast
| Feature | Calcitonin | Parathyroid Hormone (PTH) |
|---|---|---|
| Source | Thyroid C‑cells | Parathyroid glands |
| Primary effect | Lowers serum calcium | Raises serum calcium |
| Action on bone | Inhibits osteoclasts | Stimulates osteoclasts (indirectly) |
| Kidney impact | Increases calcium excretion | Decreases calcium excretion, increases phosphate excretion |
| Vitamin D interaction | Minimal | Enhances active Vitamin D synthesis |
While both hormones act on the same mineral, they do so in opposite directions. In a healthy adult, calcitonin’s effect is relatively modest compared with the powerful actions of PTH. However, its role becomes crucial during acute spikes in calcium, such as after high‑dose calcium supplements or certain medical conditions.
Clinical Situations Involving Calcitonin
Understanding calcitonin’s physiology helps explain why doctors measure it in specific scenarios.
- Hypercalcemia assessment: Excessive calcium levels can stem from malignancy, overactive parathyroid tissue, or rare endocrine tumors that also secrete calcitonin. Elevated calcitonin levels can point toward medullary thyroid carcinoma (MTC), a cancer of the C‑cells.
- Medullary thyroid carcinoma monitoring: Since MTC cells overproduce calcitonin, serial measurements serve as a tumor marker. A rising calcitonin trend often signals disease progression.
- Osteoporosis therapy: Synthetic calcitonin (e.g., salmon calcitonin) is approved in some countries for short‑term treatment of post‑menopausal osteoporosis. It modestly reduces vertebral fracture risk by dampening bone turnover.
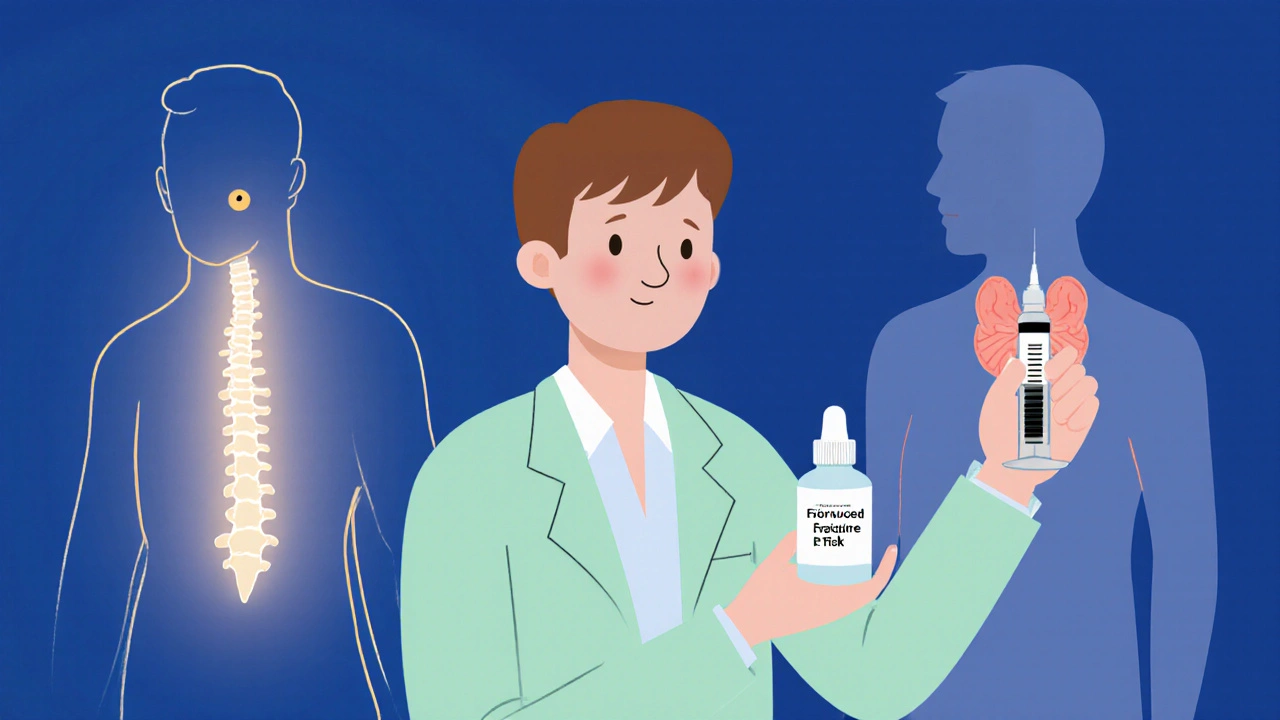
Therapeutic Use of Synthetic Calcitonin
Pharmaceutical calcitonin, usually derived from salmon because it’s more potent in humans, is administered via nasal spray or injection. Indications include:
- Acute management of hypercalcemia, especially when rapid reduction is needed.
- Pain relief in acute osteoporotic vertebral compression fractures.
- Adjunct therapy for Paget’s disease of bone, where it helps control abnormal bone remodeling.
It’s important to note that long‑term use is discouraged because tolerance can develop, and the fracture‑prevention benefit is modest compared with bisphosphonates or newer agents like denosumab.
Side Effects and Contraindications
Most patients tolerate calcitonin well, but some experience:
- Nasal irritation or epistaxis (if using a spray).
- Gastrointestinal upset such as nausea.
- Rare allergic reactions.
Calcitonin is not recommended for patients with a known hypersensitivity to the product, and caution is advised in those with severe renal impairment because the kidneys play a role in calcium excretion.
Practical Takeaways for Everyday Health
If you’re wondering whether you need to worry about calcitonin, here are the bottom‑line points:
- Calcitonin acts as a safety valve to prevent calcium overload; most healthy people never notice its effects.
- Blood tests for calcitonin are only ordered when doctors suspect medullary thyroid cancer or need to monitor known disease.
- Dietary calcium and vitamin D remain the foundation of bone health; calcitonin supplements are rarely required outside specific medical conditions.
- For osteoporosis, focus on proven therapies (bisphosphonates, denosumab, lifestyle changes) and view calcitonin as a short‑term adjunct, not a primary solution.
Future Research Directions
Scientists are exploring whether newer analogs of calcitonin could provide stronger anti‑resorptive effects without tolerance. Early animal studies suggest that combining calcitonin analogs with other bone‑building agents might synergize, but human trials are still pending as of 2025.
Key Takeaways
calcitonin is a thyroid‑derived hormone that lowers blood calcium by slowing bone breakdown, complementing the calcium‑raising actions of PTH. It has niche clinical uses in hypercalcemia, osteoporosis, and as a tumor marker for medullary thyroid carcinoma, but for most people its everyday impact is subtle.
What triggers the release of calcitonin?
A rise in serum calcium-often after a calcium‑rich meal or IV calcium infusion-stimulates the thyroid’s C‑cells to secrete calcitonin.
How does calcitonin differ from parathyroid hormone?
Calcitonin lowers blood calcium by inhibiting osteoclasts and increasing renal excretion, whereas PTH raises calcium by stimulating osteoclasts (indirectly), reducing renal excretion, and activating Vitamin D.
Is calcitonin used to treat osteoporosis?
Yes, but only for short‑term use in post‑menopausal women or men with recent vertebral fractures. Its fracture‑prevention benefit is modest compared with stronger agents.
Can a blood test for calcitonin diagnose bone disease?
Not directly. Elevated calcitonin is most useful as a marker for medullary thyroid carcinoma. Bone diseases are better evaluated with calcium, PTH, Vitamin D, and imaging.
What are common side effects of synthetic calcitonin?
Nasal irritation (spray), nausea, and rarely allergic reactions. Long‑term use can lead to tolerance, reducing its effectiveness.
Kevin Stratton
When you look at calcium regulation through a philosophical lens, calcitonin emerges as the humble guardian of balance 😊. It quietly steps in after a calcium surge, reminding the body that excess can be just as dangerous as deficiency. Think of it as the yin to PTH's yang, a subtle counter‑weight that keeps the system from tipping. Without this brake, our bones would whisper louder warnings of resorption. In the grand tapestry of endocrinology, even the quiet players matter.
Jennie Smith
Wow, such a clear breakdown! 🌟 I love how the article paints calcitonin as a safety valve – it's like having a friendly alarm system for your bones. The colorful tables make the differences from PTH pop, and the practical tips feel super actionable for anyone caring about bone health. Keep the vibes upbeat and the science solid, and we’ll all walk away a little wiser.
Anurag Ranjan
Calcitonin acts like a brake on calcium spikes.
James Doyle
The endocrine orchestra that governs mineral homeostasis is a masterpiece of physiological engineering, and calcitonin, though often relegated to the footnotes, occupies a pivotal niche in this symphony. From a mechanistic standpoint, calcitonin binds to G‑protein coupled receptors on osteoclast membranes, initiating a cascade of intracellular second messengers that culminate in the suppression of bone resorptive activity. This inhibition translates into a measurable decrement in serum calcium flux, effectively applying a negative feedback loop that curtails hypercalcemic excursions. Clinically, the therapeutic exploitation of this pathway is manifested in recombinant salmon calcitonin formulations, which boast higher receptor affinity due to evolutionary divergence. The nasal spray delivery system, while convenient, introduces mucosal considerations such as rhinitis and epistaxis, underscoring the necessity of patient selection. Intravenous injection, on the other hand, offers rapid pharmacokinetics appropriate for acute hypercalcemia, particularly in malignancy‑associated scenarios where calcium levels threaten renal and neurological function. It is imperative to recognize that the magnitude of calcitonin’s effect is dwarfed by parathyroid hormone, rendering its physiologic role more akin to a safety valve than a primary regulator. Nonetheless, in the context of osteoporotic vertebral compression fractures, calcitonin provides analgesic benefits through modulation of nociceptive pathways, a facet often overlooked in guideline discussions. The development of tolerance after several weeks of continuous exposure is a pharmacodynamic limitation that necessitates strategic drug holidays or combination therapy. Recent meta‑analyses have juxtaposed calcitonin against bisphosphonates, revealing a modest reduction in vertebral fracture incidence but an unfavourable risk‑benefit profile when adverse events are accounted for. Moreover, the biomarker utility of calcitonin in medullary thyroid carcinoma surveillance cannot be overstated; serial measurements correlate with tumor burden and therapeutic response. From a research perspective, novel analogs aim to dissociate the anti‑resorptive properties from the tachyphylaxis phenomenon, employing peptide engineering to enhance stability. Early phase trials report promising osteoclast inhibition without the classical attenuation observed with native calcitonin, hinting at a potential paradigm shift. However, regulatory hurdles and the cost‑effectiveness equation remain formidable barriers before widespread clinical adoption can be envisaged. In sum, calcitonin is a multifaceted molecule that, despite its modest homeostatic clout, offers niche therapeutic avenues that merit judicious incorporation into patient‑centred care algorithms.
Edward Brown
Some people think hormones are just biochemical footnotes, but what if the “brake” they talk about is actually a covert control mechanism orchestrated by hidden elite labs? The fact that calcitonin levels can signal a thyroid tumour feels like a backdoor warning system, doesn’t it? I’m not saying it’s a conspiracy, just that we should stay skeptical about who decides which hormones get a spotlight.
Suzanne Carawan
Oh great, another article telling us calcitonin is “just a safety valve.” As if we needed a reminder that our bodies have built‑in redundancy. Next they’ll tell us water is wet.
Donal Hinely
Look, Jennie, your sunshine‑and‑rainbow take on calcitonin is cute, but let’s not sugar‑coat the fact that the hormone’s clinical payoff is basically a footnote in most treatment guidelines. If you’re looking for real bone‑saving power, you’ll need bisphosphonates or denosumab, not a nasal spray that some people can barely tolerate.
christine badilla
James, you just turned a simple hormone overview into an epic saga that could rival a Tolkien novel! While the jargon is impressive, most of us are just trying to figure out if we should bother with a calcitonin spray after a fall. Maybe dial down the academic fireworks and give us the TL;DR?
Octavia Clahar
Edward, I get the intrigue, but let’s keep the drama in movies, not in our endocrine discussions. Calcitonin is a straightforward hormone, and while it’s useful as a tumor marker, there’s no secret agenda lurking in the lab results.
Melody Barton
Suzanne, I hear your sarcasm, but let’s not dismiss the genuine utility of calcitonin in acute hypercalcemia management. It may not be a miracle drug, yet in specific cases it can buy precious time while we address the underlying cause.
Justin Scherer
For anyone wondering when to order a calcitonin test, remember it’s primarily indicated when medullary thyroid carcinoma is on the differential or when you need to monitor known disease progression. Routine calcium panels won’t include it, so discuss with your endocrinologist if you have risk factors.
Cheyanne Moxley
Justin, thanks for the textbook answer, but let’s be real – most patients never even hear the word calcitonin unless they’re caught in a rare cancer scare. It’s like a secret menu item that only the pros know about, and most of us are left clueless.