Choosing the Right Oral Diabetes Medication
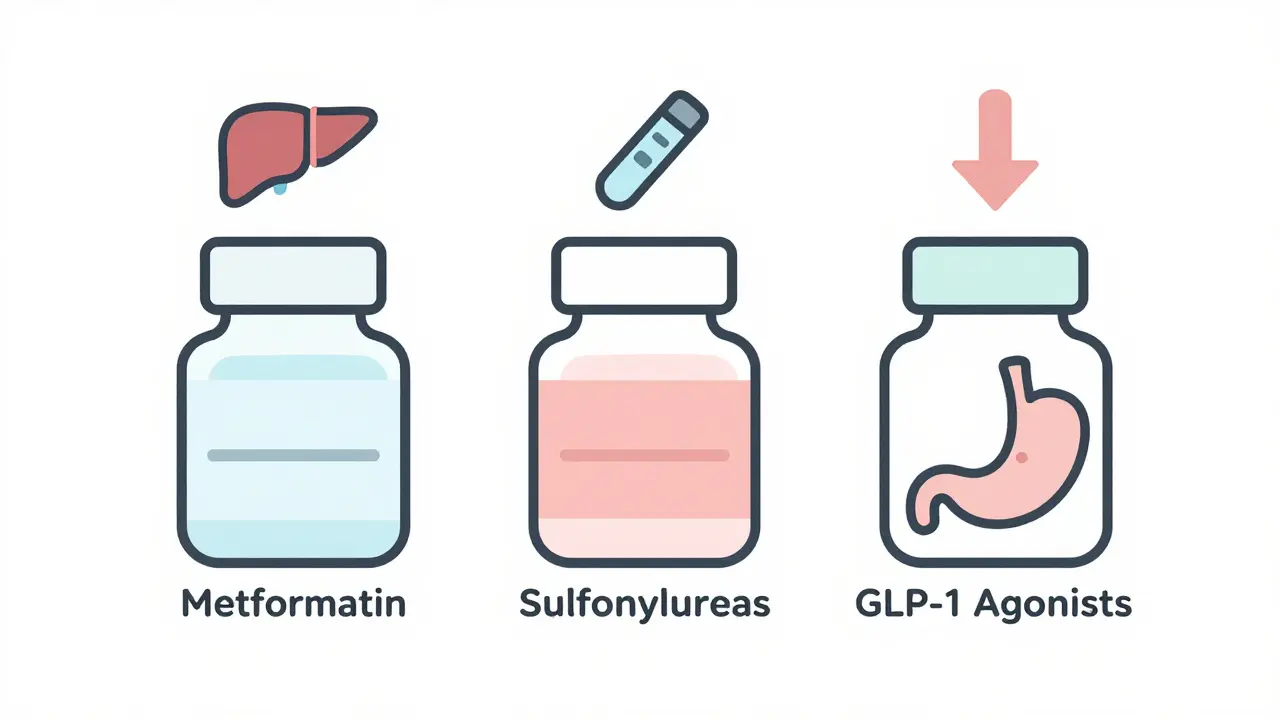
When you’re first diagnosed with type 2 diabetes, your doctor will likely hand you a prescription for metformin. It’s cheap, widely available, and has been the go-to for decades. But what if it doesn’t work for you? Or what if you’re tired of the stomach issues? Or maybe you’ve gained weight and want to lose it? That’s when you start asking: are sulfonylureas still a good option? What about those new GLP-1 agonists everyone’s talking about?
The truth is, these three classes of pills - metformin, sulfonylureas, and GLP-1 agonists - work in completely different ways. They have different side effects, different risks, and very different impacts on your weight and heart. And the choices aren’t just about lowering your A1C. They’re about how you feel every day, whether you’re scared of low blood sugar, and if you can afford the medication long-term.
Metformin: The Old Standard With New Problems
Metformin isn’t flashy. It doesn’t make headlines like Ozempic. But it’s still the most prescribed diabetes drug in the world. Over 92 million prescriptions were filled in the U.S. alone in 2023. It works by telling your liver to stop making so much glucose and helping your muscles use insulin better. On average, it drops your A1C by 1% to 2%. That’s solid.
But here’s the catch: about 20% to 30% of people can’t tolerate it. Diarrhea, bloating, nausea - these aren’t just minor inconveniences. For some, they’re deal-breakers. Even the extended-release version doesn’t help everyone. One user on a diabetes forum said, “I’ve tried every brand and dose. My stomach just won’t settle.”
Metformin doesn’t cause low blood sugar on its own. That’s a big plus. It also doesn’t make you gain weight - some people even lose a few pounds. But there’s a new concern. A 2024 study of over 2.5 million people found that those taking metformin were more than twice as likely to be diagnosed with Alzheimer’s compared to those on GLP-1 agonists. That doesn’t mean metformin causes dementia - the link isn’t proven - but it’s something doctors are watching closely.
Before starting metformin, your kidney function needs to be checked. If your eGFR is below 45, your dose needs to be lowered. Below 30, it’s usually stopped. That’s because of a rare but serious risk called lactic acidosis, especially if you’re dehydrated or sick.
Sulfonylureas: Cheap, Effective, and Risky
Sulfonylureas like glipizide and glimepiride have been around since the 1950s. They work by forcing your pancreas to pump out more insulin. That’s powerful - they can lower A1C by 1% to 1.5%. And they’re cheap. Generic versions cost as little as $4 to $10 a month.
But that insulin boost comes at a price. Your blood sugar can crash. Mild low blood sugar happens to 15% to 30% of people each year. Severe episodes - where you need help from someone else - occur in 2% to 4% of users annually. One patient on HealthUnlocked shared: “I had four ER visits because I passed out from low blood sugar. I didn’t even feel it coming.”
These drugs also make you gain weight - typically 2 to 4 kilograms. That’s the opposite of what most people with type 2 diabetes need. And they don’t protect your heart. In fact, some studies suggest they might be worse than metformin for long-term cardiovascular health.
Doctors still prescribe them, especially for older adults who can’t afford newer meds or who have trouble with injections. But they’re falling out of favor. In 2023, sulfonylureas dropped to 8.2 million prescriptions in the U.S., while GLP-1 agonists hit 12.7 million. The American College of Physicians says these drugs carry the highest hypoglycemia risk of any oral diabetes medication.
GLP-1 Agonists: The New Powerhouse (Even If It’s an Injection)
GLP-1 agonists like semaglutide (Ozempic, Rybelsus), liraglutide (Victoza), and dulaglutide (Trulicity) are the fastest-growing class of diabetes drugs. They mimic a natural hormone that tells your body to release insulin only when blood sugar is high - so they rarely cause low blood sugar. They also slow digestion, making you feel full longer.
The results? A1C drops by 0.8% to 1.5%, and most people lose 3 to 6 kilograms. Some lose more. One user reported dropping from an A1C of 7.8 to 6.2 and losing 18 pounds without changing their diet. That’s not just better glucose control - it’s life-changing.
They also protect your heart. The LEADER trial showed liraglutide reduced major heart events by 13%. Newer drugs like semaglutide and tirzepatide (a dual agonist) show even stronger results. In 2024, the ADA/EASD guidelines said these drugs should be used in patients with heart disease, kidney disease, or heart failure - even if their A1C is already under control.
The downside? Side effects. Nausea, vomiting, and diarrhea hit 20% to 40% of users, especially at first. Most people get used to it after a few weeks, but some don’t. And until 2019, all GLP-1 agonists required injections. Now, oral semaglutide (Rybelsus) is available - a pill you take on an empty stomach every morning. Adherence is 78% with the pill versus 62% with injections.
Cost is the biggest barrier. Without insurance, these drugs cost $700 to $900 a month. Most insurance plans require step therapy - you have to try metformin and sulfonylureas first. But manufacturer programs like Novo Nordisk’s Care Connections can bring copays down to $0 for eligible patients.
How They Stack Up: Side by Side
| Feature | Metformin | Sulfonylureas | GLP-1 Agonists |
|---|---|---|---|
| A1C Reduction | 1.0%-2.0% | 1.0%-1.5% | 0.8%-1.5% |
| Weight Effect | Neutral or slight loss (2-3 kg) | Gain (2-4 kg) | Loss (3-6 kg) |
| Hypoglycemia Risk | Very low | High (15-30% per year) | Very low (unless combined with insulin) |
| Cardiovascular Benefit | Neutral | Neutral or slight risk | Significant reduction in events |
| Common Side Effects | Diarrhea, nausea, bloating | Low blood sugar, weight gain | Nausea, vomiting, diarrhea |
| Typical Cost (Monthly) | $4-$10 | $10-$30 | $700-$900 (without insurance) |
| Administration | Oral, 1-2x/day | Oral, 1-2x/day | Oral (Rybelsus) or injection |
| Renal Adjustment Needed? | Yes (eGFR ≥45 for full dose) | Yes (eGFR ≥30) | Minimal (dose adjustment for dulaglutide at eGFR <30) |
What Does Your Doctor Really Want You to Know?
There’s a reason metformin is still first-line: it’s safe, cheap, and effective for most people. But guidelines changed in 2022. If you have heart disease, kidney disease, or are overweight, your doctor should now be talking to you about GLP-1 agonists - even before you try sulfonylureas.
Dr. Richard Bergenstal, a leading endocrinologist, says: “GLP-1 receptor agonists should be strongly considered as second-line therapy for patients with established cardiovascular disease.” That’s not a suggestion. It’s a recommendation backed by years of clinical trials.
And here’s something most patients don’t realize: you don’t have to choose just one. Many people take metformin plus a GLP-1 agonist. That combo lowers A1C more than either drug alone and reduces side effects compared to adding a sulfonylurea.
But if cost is a barrier, don’t give up. Ask about patient assistance programs. Some manufacturers offer free medication for up to a year. Or talk to your doctor about switching to a generic sulfonylurea if you’re not at high risk for low blood sugar.
Real-Life Choices: Who Gets What?
Let’s say you’re 58, overweight, with an A1C of 8.1, and no heart problems. Your doctor starts you on metformin. After three months, your A1C is still at 7.5. You’ve lost 2 pounds but have constant bloating. What’s next?
If you’re worried about cost, a sulfonylurea might be the next step - but you’ll need to check your blood sugar more often and learn the signs of low blood sugar. If you’re willing to invest in your long-term health, a GLP-1 agonist could drop your A1C to 6.3 and help you lose 10 pounds - with no risk of dangerous lows.
Now imagine you’re 72, on a fixed income, with mild kidney issues and no insurance. Metformin might be too hard on your stomach. A sulfonylurea could be the only affordable option - but you’d need to avoid skipping meals and carry glucose tablets.
There’s no one-size-fits-all. The best medication is the one you can take consistently, afford, and tolerate.
What’s Next for Diabetes Meds?
The future is getting more interesting. Oral GLP-1s like Rybelsus are already here. In 2023, a triple agonist called retatrutide showed A1C drops of 3.3% and weight loss of over 24% in early trials. That’s more than double what metformin can do.
And as patents expire, biosimilar GLP-1s are coming. Experts predict costs could drop by 50% within five years. That could change everything - making the most effective drugs accessible to everyone, not just the insured.
Right now, the choice isn’t just about science. It’s about your life - your budget, your fears, your daily routine. Metformin is still the baseline. Sulfonylureas are fading but still useful. GLP-1 agonists are the future - if you can get them.
Is metformin still the best first choice for type 2 diabetes?
Yes, for most people. Metformin is still the first-line recommendation because it’s effective, safe, and affordable. It doesn’t cause weight gain or low blood sugar on its own. But if you have heart disease, kidney disease, or need to lose weight, your doctor should also discuss GLP-1 agonists right away - even as a first option.
Why are GLP-1 agonists so expensive?
They’re biologic drugs, which are more complex and costly to produce than traditional pills like metformin. Patent protections also limit competition. But biosimilars are in development, and manufacturer assistance programs can cut costs to $0 for eligible patients. Insurance often requires trying cheaper meds first before approving GLP-1s.
Can I take a GLP-1 agonist if I’ve had stomach surgery?
Not usually. GLP-1 agonists slow digestion, which can cause dangerous delays in stomach emptying. If you’ve had gastric bypass, sleeve gastrectomy, or other major stomach surgery, these drugs are generally avoided. Always tell your doctor about any prior abdominal surgeries before starting.
Do sulfonylureas cause weight gain because they make you hungry?
Not directly. Sulfonylureas force your pancreas to release insulin, which lowers blood sugar. When blood sugar drops too low, your body signals hunger to raise it again. That’s why many people on sulfonylureas end up eating more - and gaining weight. It’s a side effect of the drug’s mechanism, not an appetite stimulant.
Is there a pill version of Ozempic?
Yes - it’s called Rybelsus. It’s oral semaglutide, the same active ingredient as Ozempic, but in a pill form you take once daily on an empty stomach. It’s not as strong as the injection, but it’s much more convenient. Adherence rates are higher with the pill because people don’t have to inject themselves.
Can I stop taking my diabetes meds if I lose weight?
Sometimes. Significant weight loss - especially through diet, exercise, or bariatric surgery - can put type 2 diabetes into remission. Many people reduce or stop meds. But this isn’t guaranteed. Your A1C needs to stay below 6.5% for at least 6 months without medication before your doctor considers stopping treatment. Never stop meds without medical supervision.
What to Do Next
If you’re on metformin and tolerating it - keep going. If you’re struggling with side effects, ask about the extended-release version or switching to a GLP-1 agonist. If you’re on a sulfonylurea and having low blood sugar episodes, talk to your doctor about alternatives. And if cost is stopping you from trying a GLP-1 agonist, ask about patient assistance programs - they’re more common than you think.
Your diabetes management isn’t a one-time decision. It’s a conversation that evolves with your health, your goals, and your life. The right medication isn’t the one with the best data - it’s the one you can stick with for the long haul.
Mohammed Rizvi
Metformin’s the old reliable like a pair of worn-out sneakers-comfortable until they start smelling like regret. I’ve been on it for five years. Diarrhea? Check. Weight loss? A little. Alzheimer’s risk? I’d rather lose my memory than my kidneys. Still, at $5 a month, I’ll take the side effects over the price tag of a new car.
Curtis Younker
I just want to say how amazing it is that we’re finally talking about diabetes meds like actual human beings instead of just numbers on a chart. I started on metformin, hated the stomach stuff, tried glipizide and nearly passed out at the grocery store-scary stuff-then switched to Rybelsus and my life changed. I lost 22 pounds, my A1C dropped to 5.9, and I actually feel like myself again. It’s not just about blood sugar-it’s about living. And yes, it’s expensive, but I applied for Novo’s program and got it for free. Don’t give up. There’s hope out there.
TONY ADAMS
Why do you guys even care? Just take the pill. Who cares if you lose weight or your heart gets better? I got diabetes, I take my meds, I eat what I want. If I die early, I lived hard. Metformin? Sure. GLP-1? Whatever. Just give me something that doesn’t make me cry in the bathroom.
George Rahn
The commodification of metabolic health in the neoliberal pharmaceutical state is a profound betrayal of the Hippocratic ethos. One cannot reduce the human organism to a mere algorithm of A1C values and cost-per-pill metrics. The moral imperative lies not in the pharmacological hierarchy, but in the ontological dignity of the patient who must navigate a system designed to profit from their suffering. GLP-1 agonists, while statistically superior, remain instruments of capitalist medical hegemony.
Napoleon Huere
It’s funny how we treat diabetes like a problem to be solved, when really it’s a mirror. Metformin makes you question your body. Sulfonylureas make you fear your body. GLP-1 agonists make you love your body-even if it costs a fortune. We’re not just managing glucose. We’re negotiating identity. Who are you when your pancreas fails? Are you the person who takes the cheap pill and suffers? Or the one who spends a fortune to feel alive? There’s no right answer. Only truth.
rasna saha
I was on metformin for a year and felt like my insides were rearranging themselves. Switched to Rybelsus after my doctor pushed me-was scared of the cost, but my employer’s plan covered it. Lost 15 pounds, no crashes, no panic. I just feel… lighter. Not just physically. Like I can breathe again. If you’re on the fence, talk to your doc. It’s not just a pill-it’s a reset.
Skye Kooyman
The Alzheimer’s link with metformin is weird. I read the study. Correlation isn’t causation but still. Why now? Why only in the last 2 years? What changed in the data? Also why is no one talking about how GLP-1s might protect the brain? That’s the real story
Uche Okoro
The pharmacokinetic profile of sulfonylureas exhibits a marked propensity for insulin hypersecretion, which precipitates hypoglycemic episodes via β-cell exhaustion. This is not merely a side effect-it is a pharmacodynamic liability. The 2023 ADA/EASD guidelines reflect a paradigm shift toward incretin-based therapies, which demonstrate superior cardiovascular risk mitigation and beta-cell preservation. The continued use of sulfonylureas in non-elderly, non-indigent populations constitutes clinical malpractice.
shivam utkresth
In India, metformin is the only option for most. Sulfonylureas? Rare. GLP-1s? Only for the rich or the lucky. I’ve seen patients skip meals just to avoid lows from glimepiride. One uncle died because he didn’t know his shaking meant low sugar. We need better access. Not just science-justice. The same drug that saves lives in the US kills quietly here because it’s too expensive. That’s not medicine. That’s inequality.
Aurelie L.
I tried the pill. Nausea for three weeks. Gave up. Now I’m back on metformin. My stomach hates me. My doctor says I’m lucky I don’t have heart disease. I’m not lucky. I’m tired.
bella nash
The historical precedence of metformin as first-line therapy is grounded in its extensive clinical documentation and cost-effectiveness profile. However, the emergence of GLP-1 receptor agonists with demonstrated cardiovascular and renal protective effects necessitates a reevaluation of therapeutic algorithms. The decision to deprioritize these agents based on cost alone represents a failure of healthcare policy rather than pharmacology