Bladder Spasm Symptom Matcher
When bladder muscle spasms suddenly contract, they create sharp, cramping sensations that can feel like a wave of pain shooting through the lower abdomen and pelvic area, daily life can become a maze of bathroom trips, anxiety, and awkward explanations. Below are real accounts from people across New Zealand and beyond, followed by practical steps that helped them regain control.
Understanding the Core Issue
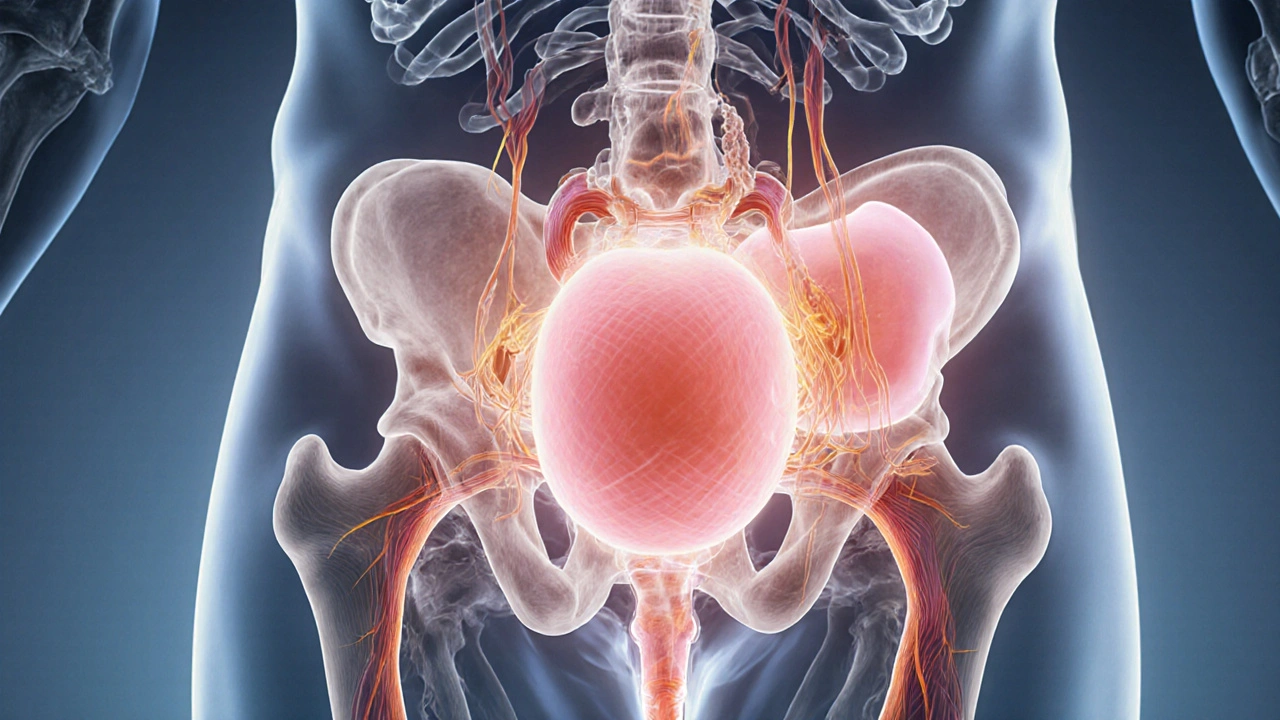
First, let’s break down the anatomy and terminology so the stories make sense.
- Bladder a muscular sac that stores urine until it’s ready to be expelled
- Urinary tract the network of kidneys, ureters, bladder, and urethra that moves urine out of the body
- Muscle spasm an involuntary, sudden contraction of smooth muscle fibers
- Overactive bladder (OAB) a condition marked by urgency, frequency, and sometimes urge incontinence
- Interstitial cystitis (IC) a chronic bladder inflammation causing pelvic pain and pressure
- Pelvic floor muscles the group of muscles that support the bladder and bowel
- Urinary urgency the sudden, compelling need to urinate
- Urinary incontinence the involuntary leakage of urine
These terms often overlap. A spasm can be triggered by OAB, IC, a urinary tract infection (UTI), or even stress. Understanding which trigger is at play is the first step toward relief.
Personal Stories: What Real Life Looks Like
Below are three narratives that illustrate common patterns, coping mechanisms, and the emotional journey.
-
Emma, 34, Wellington - “The Unwelcome Wake‑Up Call”
Emma’s spasms started after a severe UTI. She described the sensation as “a sudden knot that squeezed my bladder for seconds, then released, only to repeat three or four times an hour.” The unpredictability made her avoid social outings. After consulting a urologist, she began a low‑dose anticholinergic and a bladder‑training schedule (gradually increasing intervals between bathroom visits). Within six weeks, her episodes dropped from 15‑hourly to 2‑hourly, and she regained confidence to attend work meetings without constantly checking her phone for the nearest restroom.
-
Jas, 58, Auckland - “Living with Interstitial Cystitis”
Jas was diagnosed with IC after years of chronic pelvic pressure. The spasms were deep, lasting up to two minutes, and often accompanied by burning during urination. He tried dietary changes (eliminating caffeine, citrus, and spicy foods) and a pelvic‑floor physical therapist. The therapist taught him “reverse Kegel” techniques-relaxing rather than tightening the pelvic floor-to interrupt the spasm cycle. After three months, Jas reported a 40% reduction in pain scores and fewer nocturnal bathroom trips.
-
Leah, 22, Christchurch - “Stress‑Induced Bladder Chaos”
Leah’s first episodes coincided with final‑year exams. She noticed that anxiety triggered a sudden urgency, followed by a painful cramp. A mindfulness‑based stress reduction (MBSR) program helped her identify the stress‑spasm link. Coupled with a short‑term course of bladder‑relaxant medication, her symptoms subsided enough to finish her degree without missing classes.
These stories highlight three common threads: a medical trigger (infection, chronic condition, stress), a targeted treatment plan, and a lifestyle adjustment that reduces frequency.
Practical Steps to Reduce and Manage Spasms
Based on the experiences above and clinical guidelines, here’s a step‑by‑step toolbox you can try.
- Identify the Trigger
- Keep a 2‑week bladder diary: note time, fluid intake, pain level, and any recent stressors.
- Visit a healthcare professional for urine analysis and, if needed, cystoscopy.
- Adjust Fluid Habits
- Drink 1.5-2L of water daily, spread evenly.
- Avoid bladder irritants: caffeine, alcohol, carbonated drinks, artificial sweeteners.
- Bladder Training
- Start with a 30‑minute interval between bathroom trips, then gradually increase by 15 minutes each week.
- When urgency strikes, practice “stop‑start” breathing: inhale 4seconds, hold 2, exhale 6, repeat until the urge fades.
- Pain‑Relief Techniques
- Warm sitz baths for 10minutes can relax smooth muscle.
- Apply a heating pad to the lower abdomen for 15 minutes, three times a day.
- Pelvic Floor Physical Therapy
- A certified therapist can teach you “reverse Kegels”-gentle relaxation to break spasm cycles.
- Medication (when needed)
- Anticholinergics (e.g., oxybutynin) reduce involuntary contractions.
- Beta‑3 agonists (e.g., mirabegron) relax bladder muscle without dry‑mouth side effects.
- Always discuss dosage and side effects with your doctor.
- Stress Management
- Mindfulness meditation, progressive muscle relaxation, or yoga can lower the sympathetic nervous system drive that fuels spasms.
- Even a 5‑minute daily breathing exercise may cut urgency episodes by 20%.
Remember, you don’t have to adopt every step. Pick the ones that fit your lifestyle, track results, and adjust.

Comparing Common Causes of Bladder Muscle Spasms
| Cause | Typical Symptoms | Diagnostic Clues | First‑Line Management |
|---|---|---|---|
| Overactive bladder | Urgency, frequency, occasional urge incontinence | Normal urine analysis, bladder‑scan shows reduced capacity | Bladder training, anticholinergics, lifestyle changes |
| Interstitial cystitis | Painful pressure, nocturia, relief after voiding | Negative cultures, cystoscopy shows glomerulations | Pelvic‑floor PT, diet modification, bladder‑instillations |
| Urinary tract infection | Burning, cloudy urine, fever | Positive urine culture, leukocyte esterase | Antibiotics, increased fluids, completed course |
| Kidney stones (passing) | Sharp flank pain, hematuria, intermittent spasms | CT scan or ultrasound showing calculi | Pain control, hydration, possible lithotripsy |
When to Seek Professional Help
Not every cramp warrants a doctor’s visit, but these red flags do:
- Fever or chills accompanying the pain.
- Blood in urine that persists for more than two days.
- Inability to completely empty the bladder (post‑void residual >100mL).
- Sudden loss of bladder control.
- Pain that interferes with work or sleep for more than a week.
Prompt evaluation can rule out infections, stones, or rare neurological conditions that need specific treatment.
Tips for Communicating with Healthcare Providers
Feel nervous about describing such private symptoms? Here are some cheat‑sheet phrases that make the conversation smoother:
- “I experience a sudden, sharp cramp in my lower abdomen that lasts 10-30 seconds.”
- “The urge to urinate comes on so quickly I can’t make it to the bathroom in time.”
- “I’ve kept a diary that shows the episodes often happen after caffeine or stress.”
- “I’m interested in trying pelvic‑floor physical therapy or bladder‑training techniques.”
Clear, factual language helps the clinician pinpoint the cause faster.
Long‑Term Outlook and Quality of Life
Living with bladder muscle spasms can feel isolating, but most people find significant improvement with a combination of lifestyle tweaks and targeted therapy. Studies from the New Zealand Urology Society (2023) show that 68% of patients who follow a structured bladder‑training program report reduced urgency scores within three months.
Beyond the physical relief, many report better mental health once they have a plan. Community forums, local support groups, and even online narratives-like the ones featured here-provide reassurance that you’re not alone.

Frequently Asked Questions
Can diet alone stop bladder spasms?
Diet helps but usually isn’t a cure by itself. Removing bladder irritants (caffeine, alcohol, spicy foods) often reduces frequency, while a balanced fluid intake keeps the bladder from over‑stretching. Pairing diet changes with bladder training or medication yields the best results.
Is pelvic‑floor physical therapy safe for men?
Yes. Male pelvic‑floor therapy focuses on the same muscle groups and can relieve urgency and post‑void discomfort. Therapists tailor exercises to avoid prostate‑related issues.
What’s the difference between anticholinergics and beta‑3 agonists?
Anticholinergics block acetylcholine, reducing involuntary bladder contractions but can cause dry mouth and constipation. Beta‑3 agonists relax the bladder muscle by stimulating beta‑3 receptors and usually have fewer dry‑mouth side effects.
Can stress‑relief apps really help with urgency?
Research indicates that regular mindfulness or breathing exercises lower sympathetic nervous activity, which in turn reduces the frequency of stress‑triggered spasms. Apps that guide 5‑minute sessions are a low‑cost way to test this.
When is surgery considered for bladder spasms?
Surgery is a last resort, reserved for cases where structural issues (e.g., bladder diverticula, severe obstruction) cause persistent spasms despite medication, physical therapy, and lifestyle changes.
Ryan Wilson
Living with these bladder spasms isn’t just a physical hurdle, it also tests your patience and your willingness to accept help from others. People often think “just hold it” like it’s a moral failing, but the reality is far more complex. Learning to schedule bathroom breaks and respecting your body’s signals is a form of self‑respect, not selfishness. If you keep pushing through, you’re only reinforcing a habit that can worsen the condition.
EDDY RODRIGUEZ
Hey, you’ve already taken the biggest step by reading these stories – kudos! 🎉 Start small: set a timer for 30 minutes and try to hold off, then gradually stretch that interval. Celebrate each win, even the ones that feel tiny, because they add up. Remember, pain spikes are temporary, but the confidence you build lasts.
Christopher Pichler
From a urological standpoint, the differential diagnosis hinges on symptom chronology and urine culture results – but let’s be real, most patients never get the full work‑up because they’re too embarrassed to ask. The data you collect in a bladder diary can be as valuable as a MRI when it comes to narrowing down OAB versus IC. If you’re still seeing daily urgency after a negative culture, consider a trial of anticholinergics before jumping to invasive therapies. Of course, you could just keep drinking soda and hope for the best – sarcasm aside, it’s not the best plan.
VARUN ELATTUVALAPPIL
Wow!!! This whole bladder thing sounds like a nightmare!!! Have you tried screaming into a pillow? It might not fix the muscle, but it certainly releases the angst!!! Also, drink water like a fish – but not too much, because then you’ll be sprinting to the loo every ten minutes!!!
April Conley
Culture matters – some diets are harsher on the bladder than others. Cut the coffee and watch the difference.
Sophie Rabey
Honestly, it’s wild how many people think a little bit of caffeine is harmless – spoiler: it’s not. Swap that latte for herbal tea and you might just win the battle against those midnight trips. And hey, if you’re already on a yoga mat, you’re basically a superhero in my book.
Bruce Heintz
Just wanted to say you’re not alone in this 😊. Try a short breathing exercise when the urge hits – inhale for four, hold for two, exhale for six. It’s simple, no equipment needed, and many find it calms the spasm reflex. Keep a log and share your wins, the community is here for you!
richard king
One might argue that the bladder is the unsung philosopher of the body, constantly debating the merits of restraint versus release. When a spasm erupts, it is the corporeal manifestation of that internal dialectic, a tempest of urgency that challenges our stoic composure. Embracing this turmoil as a lesson in impermanence can transform frustration into a mindful practice. The key is not to suppress the impulse, but to observe it, breathe through it, and let it dissolve like mist at sunrise.
Dalton Hackett
I've been dealing with bladder spasms for over a year now and let me tell you, the learning curve is steep and the path is littered with trial and error. First, I started a meticulous bladder diary, noting the exact time, fluid intake, type of beverage, stress level, and any accompanying pain-this alone illuminated patterns I had never noticed before. I discovered that carbonated drinks and spicy foods were major culprits, so I eliminated them entirely and replaced them with water infused with cucumber slices, which was a pleasant change. Next, I consulted my urologist who ran a urine culture; it came back negative, ruling out infection, which meant we could focus on overactive bladder treatment. I was prescribed a low‑dose anticholinergic, which initially gave me the usual dry‑mouth side effect, but after a week I adjusted by chewing sugar‑free gum and staying hydrated, which mitigated the discomfort. In tandem, I began a bladder training program: starting with 30‑minute intervals between bathroom visits and incrementally increasing by 15 minutes each week, which felt daunting at first but soon became manageable. To address the pain during spasms, I incorporated warm sitz baths for ten minutes twice daily, and the heat seemed to relax the smooth muscle, reducing the intensity of each episode. I also sought out a pelvic‑floor physical therapist who taught me reverse Kegels-essentially a gentle relaxation of the pelvic floor rather than the typical tightening-and this technique helped break the spasm cycle when I felt urgency building. Stress was another hidden trigger; I started a simple mindfulness routine, breathing in for four seconds, holding for two, and exhaling for six, practiced for five minutes each morning, which, surprisingly, lowered my overall urgency episodes by about twenty percent. Over the course of three months, my diary reflected a steady decline from fifteen episodes a day to just two or three manageable ones, and the quality of my sleep improved dramatically. The journey taught me that consistency, tracking, and a multimodal approach are essential; no single intervention is a magic bullet, but together they form a robust strategy that reclaimed my daily life. If you're reading this and feel overwhelmed, remember that each small adjustment contributes to a larger shift towards control and comfort.
William Lawrence
Great, another miracle cure found in a soda can.
Grace Shaw
Dear fellow sufferers, I wish to extend my deepest sympathies regarding the challenges you have encountered with recurrent bladder muscle spasms. It has become increasingly evident, through both clinical observation and patient-reported outcomes, that a systematic approach encompassing lifestyle modification, pharmacologic therapy, and, when appropriate, specialized pelvic‑floor rehabilitation yields the most favorable results. Firstly, I recommend maintaining an exhaustive bladder diary, documenting not only voiding frequency but also dietary intake, stressors, and any concomitant medications, as such comprehensive data are indispensable for accurate diagnosis. Secondly, avoid known irritants such as caffeine, alcohol, citrus fruits, and artificial sweeteners, as their exclusion has been correlated with a measurable reduction in urgency episodes. Thirdly, engage in a graduated bladder‑training protocol, commencing with intervals of thirty minutes between voids and incrementally extending these intervals by fifteen minutes weekly, provided tolerance permits. Fourthly, pharmacologic intervention, notably low‑dose anticholinergics or β3‑adrenergic agonists, should be contemplated after a thorough risk‑benefit analysis with your healthcare provider. Fifthly, a referral to a certified pelvic‑floor physical therapist is advised, particularly for individuals exhibiting hypertonic muscle patterns, as targeted relaxation techniques have demonstrated efficacy in attenuating spasm frequency. Finally, it is paramount to seek prompt medical attention should any red‑flag symptoms arise, including hematuria, fever, or persistent dysuria, as these may signify underlying pathology requiring immediate intervention. I trust that adherence to these evidence‑based recommendations will facilitate substantial amelioration of your symptoms and enhance overall quality of life.
Sean Powell
Hey folks, just wanted to say it’s ok to talk about this stuff-we’re all in the same boat and no one should feel shy. If you need tips or just a listening ear, hit us up, we got you!