More than 10% of people in the U.S. say they’re allergic to penicillin. But here’s the catch: up to 90% of them aren’t. Many people outgrow their allergy, misremember a rash from childhood as an allergy, or confuse side effects like nausea or diarrhea with true immune reactions. The result? Millions are unnecessarily avoiding the safest, cheapest, and often most effective antibiotics - and instead getting stronger, more expensive drugs that can harm their gut, increase antibiotic resistance, and raise hospital bills by hundreds of dollars per admission.
What Makes a Drug Allergy Real?
Not every bad reaction to a drug is an allergy. True drug allergies involve your immune system. They’re not just side effects. They’re your body mistaking a medication for a threat and launching a response - sometimes severe. The most dangerous are immediate-type reactions, which happen within an hour of taking the drug. These include hives, swelling of the face or throat, trouble breathing, wheezing, drop in blood pressure, or anaphylaxis. Penicillin and other beta-lactam antibiotics (like amoxicillin, cefazolin, ceftriaxone) are the most common triggers. NSAIDs - think ibuprofen, naproxen, aspirin - are another major group. But here’s something surprising: NSAID allergies usually don’t work the same way as penicillin allergies. Penicillin reactions are often IgE-mediated, meaning your body makes specific antibodies that trigger mast cells to release histamine. NSAID reactions are more often pharmacological - they happen because the drug blocks certain enzymes, leading to an imbalance in inflammatory chemicals. That’s why NSAID reactions can look similar (hives, swelling) but require different testing and different desensitization approaches.Penicillin Allergy: The Most Misdiagnosed Condition in Medicine
If you’ve been told you’re allergic to penicillin, chances are you’ve been mislabeled. Skin testing is the gold standard for confirming a true penicillin allergy. It involves tiny pricks and injections of penicillin derivatives - not just the drug itself, but also major and minor determinants like PPL (penicilloyl-polylysine) and MD (major determinant). But here’s the key detail: PPL alone is unreliable. Up to 70% of people who react only to PPL can safely take penicillin later. That’s why experts now recommend testing with both major and minor determinants, followed by a drug challenge if skin tests are negative. A negative skin test? Then you’re given a full dose of amoxicillin under supervision. If you don’t react, you’re not allergic. Period. This isn’t just theory - it’s practice. Hospitals that do this routinely find that 95% of patients labeled penicillin-allergic can safely take penicillin after testing. And when they do, their infections clear faster, they’re less likely to get resistant infections like C. diff, and their hospital stays are shorter.NSAID Allergies: More Complex Than They Appear
NSAID allergies are trickier. Unlike penicillin, there’s no reliable skin test or blood test for them. Diagnosis is based on history - did you get hives or swelling within an hour of taking aspirin or ibuprofen? Did it happen every time? Did you have asthma or nasal polyps along with it? That last part matters. People with Samter’s Triad (asthma, nasal polyps, and NSAID sensitivity) have a unique, lifelong intolerance that requires long-term management. For those with confirmed NSAID allergy, desensitization isn’t just an option - it’s often the only way to keep using essential pain relief or prevent heart attacks (if you need daily aspirin). The protocol is different from penicillin. Instead of a 4- to 8-hour IV process, it’s usually oral and slower. You start with 30 mg of aspirin, then increase every few hours: 60 mg, 100 mg, 150 mg, then 325 mg. It can take a full day. But once you’re desensitized, you can take daily aspirin without reaction - as long as you take it every day. Stop for more than 48 hours, and you lose tolerance. You’ll need to go through the whole process again.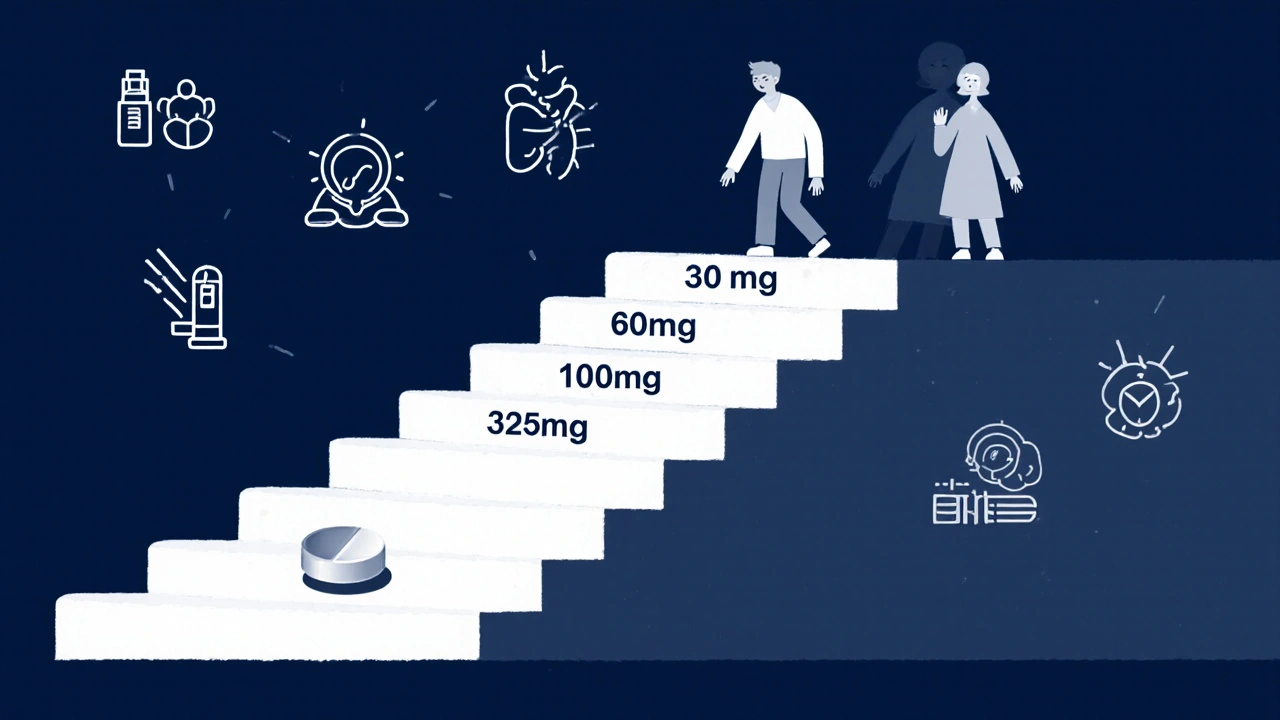
Desensitization: How It Works and When It’s Needed
Desensitization isn’t a cure. It’s a temporary override. Your immune system is tricked into tolerating the drug - just for that one treatment. Once you stop the drug, the tolerance fades. You’ll need to go through it again if you need the same drug next time. The process is carefully controlled. For IV drugs like penicillin or chemotherapy agents, you start with a dose so tiny it’s 1/10,000th of the full amount. Every 15 to 20 minutes, you get a slightly bigger dose - doubling or tripling each time - until you reach the full therapeutic level. This can take 4 to 8 hours. For some beta-lactams, like cefazolin, an accelerated 2-hour and 15-minute protocol has been proven safe and effective. You need to be in a hospital or specialized clinic. Emergency equipment - epinephrine, oxygen, IV fluids - must be immediately available. Nurses and doctors must be trained to spot early signs of reaction: flushing, itching, throat tightness, a drop in blood pressure. If things get serious - like laryngeal edema or uncontrolled low blood pressure - the process stops. No exceptions.Who Gets Desensitized? Not Everyone
Desensitization isn’t for every allergic person. It’s only done when:- You have a confirmed immediate-type reaction (within an hour) to a drug
- There’s no safe, effective alternative
- The drug is critical - like penicillin for a life-threatening infection, or paclitaxel for cancer

Children and Desensitization: The Gap in Care
Most desensitization protocols were designed for adults. Kids? They’re often treated with the same rules - even though their immune systems work differently. A 2019 review found that pediatric allergists rarely have clear guidelines for desensitizing children with drug allergies. Yet kids with chronic infections, cancer, or cystic fibrosis need these drugs too. The good news? Desensitization works in children. The bad news? Few hospitals have pediatric-specific protocols. That’s why experts say allergists need to team up with infectious disease doctors and oncologists - especially in children’s hospitals. Without that collaboration, kids get stuck with broader antibiotics or delayed treatments.The Bigger Picture: Why This Matters Beyond One Patient
When we mislabel penicillin allergies, we don’t just hurt the individual. We hurt the system. Hospitals use more expensive, broader-spectrum antibiotics. That leads to more drug-resistant infections. It increases costs. It worsens outcomes. A single mislabeled allergy can add $500 or more to a hospital bill - and that’s just for one admission. More than that, it’s a failure of diagnostics. We’ve treated penicillin allergy like a label you get at age 5 and never question. But allergies change. Immune systems adapt. What was dangerous at 8 might be harmless at 38. The solution isn’t more drugs. It’s better testing. More skin tests. More drug challenges. More desensitization programs. And more training for doctors who don’t specialize in allergies - because most patients never see an allergist. Their primary care doctor, ER physician, or oncologist needs to know when to refer, when to test, and when to consider desensitization.What You Should Do If You Think You’re Allergic
If you’ve been told you’re allergic to penicillin or an NSAID, here’s what to do:- Write down exactly what happened - symptoms, timing, how many times it occurred
- Ask your doctor: “Was this tested? Was it a true allergy, or just a side effect?”
- If you’ve never been tested, ask for a referral to an allergist
- Don’t assume you’re allergic forever - especially if it happened decades ago
- If you need a drug like penicillin or aspirin for a serious condition, ask about desensitization
Can you outgrow a penicillin allergy?
Yes, many people do. Studies show that up to 80% of people who had a penicillin allergy in childhood lose it within 10 years. Even if you had a severe reaction as a kid, you might still be able to take penicillin safely as an adult - if you get tested. Skin testing and a drug challenge are the only reliable ways to know for sure.
Is a rash always a sign of penicillin allergy?
No. Many rashes from penicillin are not allergic. They’re viral rashes that happen to appear while you’re taking the drug - especially in kids with mononucleosis or other infections. A true allergic rash is usually itchy, raised, and appears within hours of taking the drug. Non-allergic rashes are often flat, not itchy, and appear days later. Only a specialist can tell the difference.
Can you desensitize to NSAIDs like ibuprofen?
Yes, but only under strict medical supervision. Desensitization to NSAIDs is usually done with aspirin, starting at very low doses and slowly increasing. It’s not a one-time fix - you have to take the drug daily to maintain tolerance. If you stop for more than 48 hours, you’ll need to start over. This is mainly used for people who need daily aspirin for heart health or those with Samter’s Triad.
Is desensitization safe?
When done correctly, yes. Desensitization has a high success rate - over 90% for penicillin and many chemotherapy drugs. But it’s not risk-free. Reactions can happen during the process. That’s why it’s only done in hospitals with emergency equipment and trained staff. The procedure is stopped immediately if there’s any sign of a serious reaction.
Why don’t more doctors offer desensitization?
Because most doctors aren’t trained in it. Allergy specialists know the protocols, but primary care doctors, ER staff, and even oncologists often don’t. There’s also a lack of standardized guidelines, especially for kids. But awareness is growing. Hospitals like Brigham and Women’s have published clear protocols, and more institutions are starting desensitization programs - especially for cancer and infection cases where alternatives are limited.
Sameer Tawde
This is wild-so many people think they’re allergic to penicillin just because they got a rash as a kid. I had a cousin who got hives after amoxicillin at 6 and was told never to take it again. Turned out she was fine at 28 after testing. Saved her thousands in hospital bills. Why isn’t this common knowledge?
Jeff Hakojarvi
man i had no idea most of these 'allergies' are just misdiagnosed. i thought if you got a rash you were done for. my grandma got penicillin for pneumonia last year and they gave her vancomycin because she 'allergic'-turns out she never had a real reaction, just a stomach bug. she was on antibiotics for 10 days instead of 5. so dumb. why dont docs just test people first?
Timothy Uchechukwu
you people are too trusting of big pharma and their fancy tests. why do you think they want you to get skin tested? so they can sell you more drugs later. the real reason they push penicillin is because it's cheap and they control the supply. you think your body is wrong? maybe your body knows better than some doctor with a clipboard
Ancel Fortuin
desensitization? sounds like a cult ritual. next they'll tell us to drink bleach to 'build tolerance' to chlorine. they're just trying to get you hooked on drugs. what if you die during the process? who pays for that? not the hospital. not the doctor. you. and your family. this is medical theater wrapped in science jargon
Hannah Blower
the real tragedy here isn't the misdiagnosis-it's the epistemological collapse of modern medicine. we've replaced clinical judgment with algorithmic labeling. penicillin allergy becomes a data point, not a lived experience. we've commodified immunity. the body is reduced to a spreadsheet. and yet we're surprised when outcomes worsen? this isn't healthcare-it's actuarial science with a stethoscope
Gregory Gonzalez
Oh wow. So the solution to ‘I got a rash once’ is to inject me with the thing that made me break out? Brilliant. Next up: ‘I sneezed after eating peanuts, so let’s feed them to me in increasing doses until I pass out.’ Classic medical arrogance. Who approved this? A pharmaceutical lobbyist with a PhD?
Ronald Stenger
we dont need more testing. we need more discipline. if you're allergic, you're allergic. period. why are we bending over backwards to reclassify people who can't even remember what happened 20 years ago? this is just another way for lazy patients to avoid responsibility. stop blaming the system. take your damn vancomycin and be grateful you're alive
Samkelo Bodwana
look, i get the frustration. i grew up in a place where doctors didn't even have access to skin tests. we just assumed allergies were permanent. but i've seen people die because they were denied the right antibiotic. i've also seen people get sick because they took something they thought was safe but wasn't. the truth is somewhere in the middle. testing isn't perfect, but it's better than guessing. and desensitization? it saved my brother's life when he needed chemo. he was terrified. we were all terrified. but it worked. not because doctors are gods, but because they listened. and that's what matters. not the label. not the fear. just the person
Duncan Prowel
It is a matter of considerable concern that the prevalence of self-reported penicillin allergy remains so elevated in clinical practice, despite robust evidence demonstrating the high rate of false positives. The failure to implement systematic allergy evaluation protocols constitutes a systemic deficiency in primary and secondary care pathways. One might posit that the absence of standardized referral mechanisms, coupled with a paucity of allergist availability, engenders a culture of therapeutic inertia. It is imperative that institutional guidelines be revised to mandate preoperative or pre-admission allergy screening, particularly in high-risk populations. Without such intervention, the perpetuation of suboptimal antibiotic stewardship will continue to exert a deleterious effect on public health outcomes.
Bruce Bain
so if you got sick after penicillin as a kid, you might be fine now? i didnt know that. my aunt always said no penicillin, ever. she's 72. maybe she should get tested. why dont they just tell people this? its like nobody talks about it. simple stuff, but nobody says it. thanks for explaining it clear
benedict nwokedi
Of course the FDA and AMA are promoting this… because they’re complicit in the pharmaceutical-industrial complex’s agenda to normalize invasive, profit-driven ‘desensitization’ protocols. Who funds these studies? Who profits from the repeat visits? Who owns the testing kits? And why is it that the only people who benefit are the ones selling the drugs? Wake up. This isn’t medicine-it’s a multi-billion-dollar confidence trick disguised as science.
deepak kumar
i saw this in india too. people avoid penicillin because their mom said 'it made you sick when you were 5'. but in rural clinics, they use amoxicillin all the time. no problems. the real issue? no access to allergists. you need to go to a big city. and even then, they charge like it's a luxury. we need mobile testing units. not more jargon. more action.
Dave Pritchard
if you're reading this and you think you're allergic to penicillin-please don't just accept it. ask your doctor. get tested. it's safe. it's simple. and it could change your life. i've seen it happen. you don't have to live with a label from 20 years ago. you're not broken. you're just misinformed. and that's fixable.
kim pu
so basically they want us to take the drug that made us puke and break out… again? lol. next they’ll say ‘oh you hate broccoli? just eat it every day till your taste buds give up.’ i’m not falling for that. if it made me feel like death, why the hell would i want to re-expose myself? this is just corporate medicine trying to sell more pills. i’d rather take the ‘worse’ antibiotic and live with side effects than risk my life for a ‘protocol’
malik recoba
my dad had a rash after penicillin when he was 12. he’s 68 now. never took it again. last year he got a bad infection and they gave him something else. it worked, but he was sick longer. i asked him if he ever got tested. he said ‘no point, i’m old now.’ i told him it’s not about age. it’s about safety. he’s gonna get tested next week. thanks for this. really.