Bone Density Progress Calculator
Estimate your expected bone density improvement after pheochromocytoma surgery based on your initial bone density measurement.
Important Note: This calculator estimates potential bone density improvement based on clinical studies. Individual results may vary. Always discuss your bone health with your endocrinologist.
Key Takeaways
- Excess catecholamines from a pheochromocytoma can accelerate bone loss and raise fracture risk.
- Bone density testing (DXA) and blood work should be part of the routine work‑up for anyone diagnosed with an adrenal tumor.
- Managing hypertension, correcting vitamin D deficiency, and using calcium‑rich nutrition can blunt the negative impact on bones.
- Surgical removal of the tumor often stabilises bone turnover, but lifelong monitoring may still be needed.
- Patients with a history of pheochromocytoma should discuss a personalized bone‑health plan with their endocrinologist.
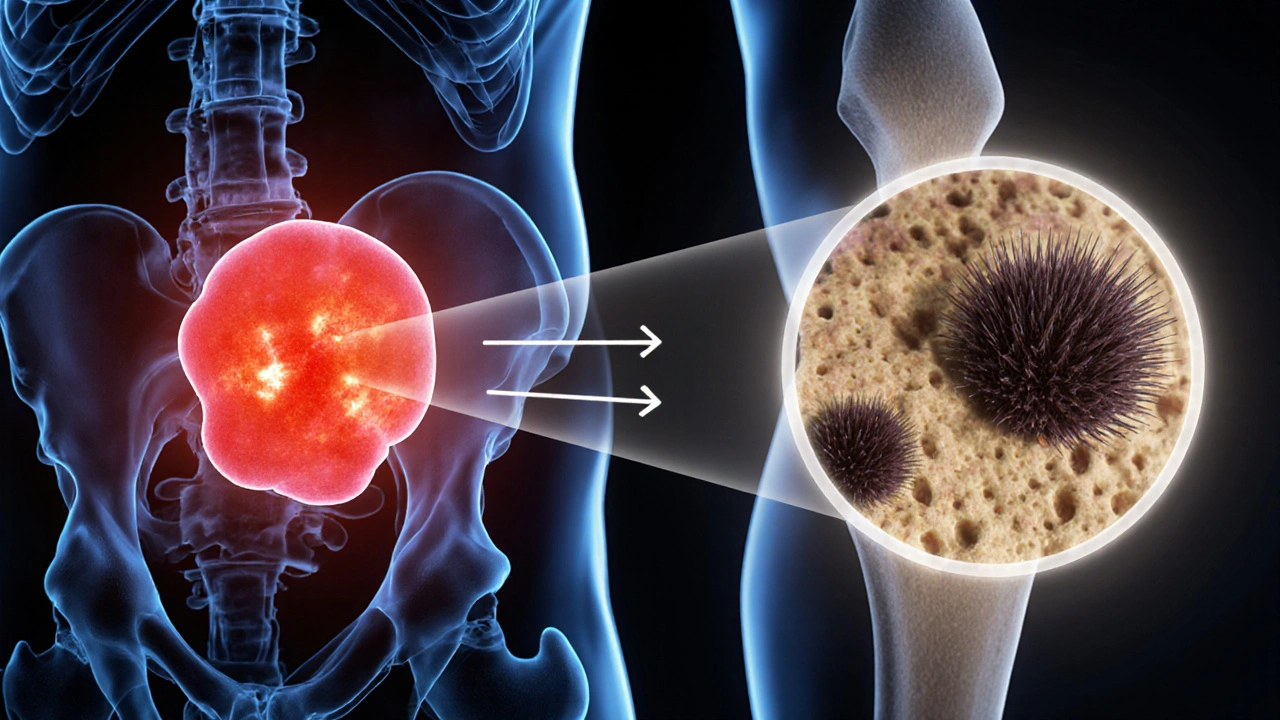
When an pheochromocytoma is described, it is an rare, usually benign tumor that arises from the chromaffin cells of the adrenal medulla and secretes large amounts of catecholamines such as adrenaline and noradrenaline. While most people hear about the classic symptoms-spikes in blood pressure, sweating, and palpitations-few realise that the hormone surge can also sabotage bone health. This article breaks down the science, shows how doctors assess risk, and offers practical steps you can take to keep your skeleton strong while you treat the tumor.
Why a Tumor in the Adrenal Gland Touches Your Bones
All bones are living tissue, constantly remodeling through the actions of osteoclasts (which break down bone) and osteoblasts (which build new bone). A delicate hormonal balance keeps this process in check. In pheochromocytoma, the flood of catecholamines does three things that tip the scale toward loss:
- Direct stimulation of osteoclasts: Laboratory studies in 2023 showed that norepinephrine binds to β2‑adrenergic receptors on osteoclast precursors, accelerating their maturation and activity.
- Increase in urinary calcium excretion: Catecholamine‑driven hyper‑adrenergic states raise renal calcium loss, leading to a subtle drop in serum calcium that triggers secondary hyperparathyroidism.
- Interference with vitamin D metabolism: Chronic high cortisol, often seen alongside catecholamine excess, reduces the conversion of 25‑hydroxy‑vitamin D to its active form, 1,25‑dihydroxy‑vitamin D.
These mechanisms converge into a net loss of bone mineral density (BMD). Population‑based data from the International Society for Endocrine Tumors (ISET) in 2024 reported that 28% of patients with untreated pheochromocytoma had osteopenia, and 12% met the diagnostic criteria for osteoporosis-rates almost three times higher than age‑matched controls.

Spotting the Hidden Bone Risks
Because bone loss can be silent, clinicians look for indirect clues. Common red flags include:
- Unexplained height loss or a new kyphotic posture.
- History of low‑impact fractures, especially in the wrist, hip, or vertebrae.
- Persistent fatigue or muscle weakness that doesn’t improve after blood pressure control.
When any of these appear alongside the classic pheochromocytoma signs, the doctor should order a bone health panel.
How Doctors Evaluate Bone Health in Pheochromocytoma Patients
The evaluation follows a two‑track approach: imaging for bone density and laboratory tests for calcium‑related hormones.
| Tool | What It Measures | Pros | Cons |
|---|---|---|---|
| DXA Scan (Dual‑Energy X‑ray Absorptiometry) | BMD at lumbar spine, hip, and forearm | Low radiation, widely available, predicts fracture risk | Cannot assess bone quality; may miss micro‑architectural changes |
| Quantitative CT (QCT) | Volumetric BMD and trabecular/cortical separation | Three‑dimensional view, better for vertebral assessment | Higher radiation, higher cost |
| Serum Markers (Calcium, PTH, 25‑OH‑vitamin D, Bone‑specific ALP) | Biochemical activity of bone turnover | Fast, useful for monitoring treatment response | Values can fluctuate; needs standardised timing |
In practice, most endocrinology clinics start with a DXA scan and a basic serum panel (total calcium, ionised calcium, parathyroid hormone, 25‑hydroxy‑vitamin D). If results are borderline, a repeat DXA in 12‑18months or a QCT for the spine can refine the risk estimate.
Protecting Your Bones While Treating the Tumor
Addressing bone health is a three‑pronged effort: control the tumor, correct metabolic imbalances, and adopt lifestyle measures.
1. Tumor Control
Most patients undergo surgical excision-laparoscopic adrenalectomy-once they are stabilised on alpha‑blockers (e.g., phenoxybenzamine) and, if needed, beta‑blockers. Studies from 2022‑2025 show that BMD stabilises in 71% of patients within six months post‑surgery, provided catecholamine levels normalize.
2. Metabolic Corrections
- Calcium & Vitamin D: Aim for serum calcium 8.5‑10.2mg/dL and 25‑OH‑vitamin D >30ng/mL. Oral calcium carbonate 500‑1000mg daily plus vitamin D3 1000‑2000IU is a common regimen.
- Parathyroid hormone (PTH) monitoring: If secondary hyperparathyroidism persists after tumour removal, a low‑dose calcitriol (0.25‑0.5µg) may be added.
- Bisphosphonates or denosumab: Reserved for those who already meet osteoporosis thresholds (T‑score ≤‑2.5) or have a recent fragility fracture.
3. Lifestyle & Physical Activity
Weight‑bearing exercises (walking, resistance training) performed for at least 30minutes on most days boost osteoblast activity. Limit excessive caffeine and alcohol, which can further increase calcium loss.

Follow‑Up: Staying on Top of Bone Health After Surgery
Even after the tumor is gone, the bone‑loss process may linger for months. A practical monitoring schedule looks like this:
- Month0-3: Re‑check catecholamine levels, serum calcium, PTH, and vitamin D. No DXA needed yet unless a fracture occurred.
- Month6: First post‑operative DXA scan to gauge any improvement.
- Month12: Repeat DXA and serum panel. If BMD has risen ≥2%, continue current regimen; if not, discuss bisphosphonate therapy.
- Year2 and beyond: Annual DXA and labs, or sooner if new symptoms arise.
Open communication with your endocrinologist is crucial. Ask about the target calcium‑vitamin D range, the need for repeat imaging, and when to consider anti‑resorptive medication.
Quick Checklist for Patients
- Ask your doctor for a baseline DXA scan at diagnosis.
- Request serum calcium, PTH, and vitamin D levels before surgery.
- Start calcium‑vitamin D supplementation if levels are low.
- Engage in weight‑bearing activity at least three times a week.
- Schedule a follow‑up DXA at 6months post‑surgery.
Frequently Asked Questions
Can pheochromocytoma cause osteoporosis on its own?
Yes. The chronic excess of catecholamines accelerates bone resorption and can lower vitamin D activation, leading to osteoporosis even before any surgical treatment.
Do I need a bone‑health specialist if I’m already seeing an endocrinologist?
Often the endocrinologist handles the initial assessment, but if the DXA shows severe loss (T‑score ≤‑2.5) or you have a fracture, a referral to a rheumatologist or osteoporosis clinic is wise for advanced therapy.
Is it safe to take calcium supplements while on alpha‑blockers?
Calcium does not interfere with alpha‑blockers. In fact, correcting calcium deficiency helps stabilise blood pressure and reduces the risk of post‑operative hypocalcemia.
How often should I repeat my DXA scan?
The typical schedule is at diagnosis, then at six months after tumor removal, and annually thereafter. If your BMD is stable, some doctors may extend the interval to two years.
Can lifestyle changes really make a difference?
Absolutely. Regular weight‑bearing exercise can increase spine BMD by up to 2% per year, and adequate calcium‑vitamin D intake is essential for the bone‑building response after the tumor is cured.
Avinash Sinha
Wow, reading about pheochromocytoma and bone health felt like stepping onto a roller‑coaster of adrenaline and calcium! The way excess catecholamines wreak havoc on osteoclasts is nothing short of apocalyptic drama. Imagine your bones as a fortress under siege, and the tumor as a relentless artillery barrage. Thankfully the article hands us the blueprints for fortifying that fortress with vitamin D, calcium, and weight‑bearing workouts. It’s a battle we can win if we arm ourselves with knowledge and perseverance.
ADAMA ZAMPOU
It is of paramount importance to recognize the systemic ramifications of pheochromocytoma beyond its classic hemodynamic manifestations. The mechanistic elucidation regarding β2‑adrenergic stimulation of osteoclastogenesis warrants further scholarly exploration. Moreover, the recommended surveillance schedule aligns with evidence‑based protocols delineated in recent endocrine guidelines. One must, however, remain vigilant for inter‑individual variability when interpreting DXA outcomes.
Liam McDonald
Great info on the bone risks.
Adam Khan
First, let me address the glaring lack of precision in the lay‑person’s description of catecholamine‑induced osteoclast activation. While the article mentions "direct stimulation," it omits the crucial downstream cAMP–PKA signaling cascade that culminates in increased RANKL expression. Second, the suggested improvement rate of 0.2 per month is a gross oversimplification; recent meta‑analyses indicate a non‑linear trajectory with an initial plateau phase lasting approximately three months post‑resection. Third, the calculator fails to account for confounding variables such as baseline vitamin D status, renal calcium handling efficiency, and concurrent glucocorticoid therapy, all of which can significantly modulate bone turnover.
Furthermore, the recommendation to commence calcium carbonate at 500‑1000 mg daily neglects the nuance that calcium carbonate requires an acidic gastric environment for optimal absorption, a condition not guaranteed in patients on proton‑pump inhibitors. A more bioavailable option would be calcium citrate, especially in the postoperative setting where gastric acidity may be altered.
In terms of imaging, the reliance on DXA alone is insufficient for detecting microarchitectural deterioration. Incorporating high‑resolution peripheral quantitative computed tomography (HR‑pQCT) can reveal trabecular density deficits that DXA masks.
Lastly, the article’s tone implies that surgical excision universally stabilizes bone mineral density within six months. This assertion disregards the subset of patients with persistent hyperparathyroidism secondary to prolonged catecholamine exposure, who may require adjunctive anti‑resorptive therapy. In summary, while the piece provides a useful overview, the clinical algorithm it proposes lacks the granularity demanded by evidence‑based endocrinology.
rishabh ostwal
One must not be lulled into complacency by the comforting statistics presented. Although 71% of patients experience BMD stabilization, the remaining 29% are left to battle progressive osteoporosis despite tumor resection. This is precisely why a proactive, not reactive, approach to calcium and vitamin D supplementation is ethically obligatory. Moreover, blind reliance on postoperative DXA without considering secondary hormonal dysregulation borders on negligent practice.
Kristen Woods
Honestly this article is a masterpiece of medical drama-so many bold claims, some of which are downright shaky. The typo in "caco___" could have been avoided, and the over‑assertive tone makes it feel like a sales pitch for supplements. Still, the core advice about weight‑bearing exercise is spot on.
Carlos A Colón
Oh sure, because nothing says "I'm concerned about your health" like a terse reminder to take calcium. Yet, the sarcasm in that line actually hides a genuine empathy for patients terrified of fractures after surgery. Remember, folks, a balanced diet and a bit of humor can go a long way when dealing with endocrine chaos.
Aurora Morealis
Good overview. The guidelines are clear A baseline DXA and vitamin D labs are essential. Follow the schedule and you’ll be fine.
Sara Blanchard
This piece does a wonderful job of bridging the gap between complex endocrine pathology and everyday patient care. By highlighting culturally sensitive communication-like explaining catecholamine effects in lay terms-we empower diverse populations to engage actively in their treatment plans. Inclusive education ultimately leads to better adherence and outcomes.
Anthony Palmowski
Alright folks, let’s cut the fluff-excess catecholamines = bone breakdown! The article’s calculator is a neat gimmick, but you can’t replace a proper endocrine work‑up with a spreadsheet! Make sure you get your labs, your DXA, and if you’re still losing bone after surgery, talk bisphosphonates with your doc! Stop waiting for miracles and start demanding concrete data!
Jillian Rooney
It’s shocking how many patients ignore the bone health warnings after pheochromocytoma surgery. The article forgets to stress that even low‑grade tumours can leave a lasting imprint on calcium metabolism. If you think you’re safe because the tumor is gone, think again-monitor your BMD relentlessly.
Rex Peterson
In reflecting upon the philosophical dimensions of endocrine disruption, one discerns a profound metaphor: the tumor as an unbidden philosopher, questioning the very foundation of skeletal integrity. This discourse invites a deeper contemplation of how systemic imbalances reverberate through the corporeal form, urging clinicians to adopt a holistic paradigm that transcends mere biochemical correction.
Candace Jones
Everyone, remember that consistent calcium (1,000 mg) and vitamin D (2,000 IU) intake, combined with three weekly weight‑bearing sessions, can add up to a measurable BMD gain within a year. If you’re unsure where to start, ask your endocrinologist to refer you to a certified exercise physiologist-personalized plans make a world of difference.
Robert Ortega
I appreciate the balanced tone of the article; it presents both the risks and the actionable steps without alarmism. Maintaining an open dialogue with your healthcare team fosters trust and better adherence to follow‑up schedules.
Elizabeth Nisbet
Just a quick heads‑up: if you feel any new bone pain after surgery, get a scan ASAP. Early detection of fractures can keep you out of the hospital.
Sydney Tammarine
Honestly, this article reads like a high‑brow manifesto on bone health-so pretentious! But hey, if you love a good dramatized science lecture, grab your popcorn and a calcium tablet 🍿💊.