When you’re undergoing chemotherapy, every pill, supplement, or even a glass of grapefruit juice can change how your treatment works. It’s not just about the cancer drug itself - it’s about what else is in your body. Chemotherapy drug interactions are one of the most overlooked dangers in cancer care, and they can turn a life-saving treatment into a life-threatening one.
Why Chemotherapy Interactions Are More Dangerous Than You Think
Most people know chemotherapy is powerful. But few realize how easily other substances can interfere with it. Unlike regular medications, chemo drugs are designed to kill fast-growing cells - including your healthy ones. That’s why even small changes in how they’re absorbed, broken down, or cleared from your body can have big consequences. Studies show over half of outpatient cancer patients experience at least one potential drug interaction. One in three of those interactions is serious enough to cause kidney damage, liver failure, or even death. In fact, research from 2001 found that drug interactions may be responsible for up to 4% of deaths in hospitalized cancer patients. That’s not a small number - it’s more than the death rate from many common infections. The problem gets worse with age. People over 65, who make up 60% of all cancer diagnoses, often take five or more medications. Their liver and kidneys don’t work as well. Their bodies process drugs slower. And they’re more likely to be taking supplements, painkillers, or heart medications that can clash with chemo.The Three Types of Interactions You Need to Know
Not all interactions are the same. There are three main types, and each one works differently:- Pharmacokinetic interactions - These affect how your body absorbs, breaks down, or gets rid of the drug. The most common type involves the CYP450 enzyme system, especially CYP3A4. This enzyme is like a factory that processes over 70% of all drugs. If something blocks or speeds up this factory, your chemo levels can spike or drop dangerously. Grapefruit and Seville oranges are big offenders - they contain compounds that shut down CYP3A4, causing chemo drugs like docetaxel or paclitaxel to build up in your blood. One grapefruit can affect your system for days.
- Pharmacodynamic interactions - These happen when two drugs affect the same part of your body in a way that makes the effect stronger or weaker. For example, combining cisplatin with another kidney-damaging drug like NSAIDs (ibuprofen, naproxen) can lead to acute kidney failure. Or, if you’re taking a blood thinner like warfarin and also use garlic, ginger, or fish oil, your risk of bleeding skyrockets during chemo.
- Immunological interactions - This is the newest and least understood danger. With immunotherapy drugs like pembrolizumab or nivolumab, your immune system is turned up to fight cancer. But if you’re also taking other drugs that affect immunity - even something as simple as an antibiotic - your body can overreact. There are documented cases of patients developing severe liver damage or skin reactions like Stevens-Johnson Syndrome after combining checkpoint inhibitors with other medications.
Supplements Are Not Safe Just Because They’re Natural
You’ve probably heard that supplements are harmless. That’s a myth - especially when you’re on chemo. The VA Whole Health Library warns that supplements aren’t regulated like drugs. Labels can be wrong. Products can be contaminated. And many contain active ingredients that interfere with chemotherapy. Here are some of the most dangerous ones:- Garlic, ginger, ginkgo biloba - Increase bleeding risk, especially before surgery or with blood thinners.
- St. John’s Wort - Speeds up CYP3A4, causing chemo drugs to break down too fast. This can make your treatment useless.
- Turmeric (curcumin) - Can interfere with drugs like doxorubicin and cyclophosphamide. It may reduce their cancer-killing effect.
- Vitamin E, fish oil, flaxseed - Raise bleeding risk. Often taken for heart health, but dangerous with chemo.
- Dong quai, black cohosh, licorice - Can affect hormone-sensitive cancers like breast or prostate cancer.
Oral Chemo Is Changing the Game
Twenty years ago, most chemo was given in the hospital through an IV. Today, about 25% of chemotherapy drugs are taken as pills - and that number is growing. Oral chemo drugs like capecitabine, lenalidomide, or abiraterone are convenient. But they’re also harder to control. When you take a pill at home, you’re responsible for timing, food, and other medications. A missed dose. A snack with grapefruit. A painkiller you grabbed without asking your doctor. These small choices can throw off your entire treatment. And because oral chemo is newer, doctors often don’t have as much data on how it interacts with other drugs. That’s why pharmacists are now playing a bigger role in cancer care. At Cancer Treatment Centers of America, pharmacists review every patient’s full medication list - including supplements, OTC drugs, and even herbal teas - before treatment starts.What You Should Do Right Now
You don’t need to be a scientist to protect yourself. Here’s what works:- Make a complete list of everything you take. Include prescription drugs, over-the-counter meds (like aspirin or antacids), vitamins, herbs, teas, and even CBD oil. Write down the dose and how often you take it.
- Bring this list to every appointment. Don’t assume your oncologist knows what you’re taking. Many patients forget to mention supplements because they think they’re “not real medicine.” They are.
- Ask your pharmacist to check for interactions. Most hospitals have oncology pharmacists who use tools like Lexicomp or Micromedex to scan your meds for risks. Ask for this service - it’s free and lifesaving.
- Avoid grapefruit, Seville oranges, and pomelos. These aren’t just “best avoided” - they’re dangerous. Even one serving can interfere with your chemo for days.
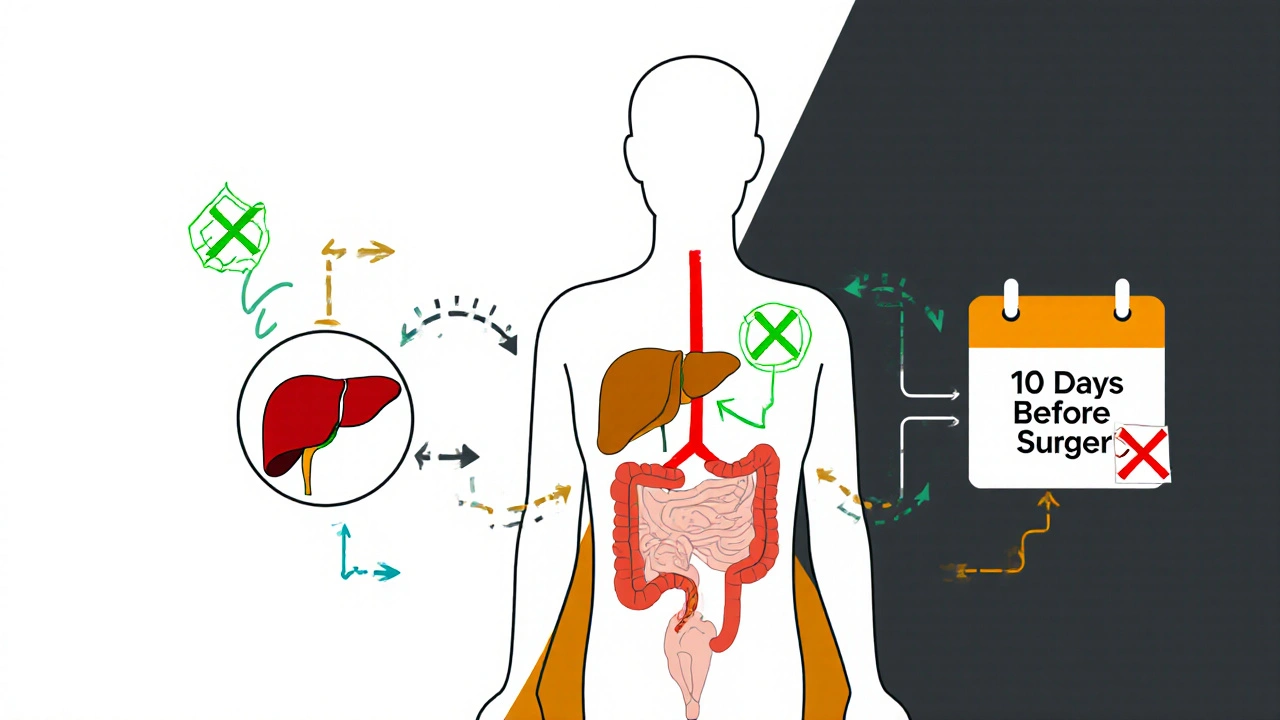
- Stop all supplements 10 days before surgery. Bleeding risks are real. Your surgical team needs to know what you’re taking.
- Don’t start anything new without asking. That includes new pain relievers, sleep aids, or “immune boosters.” If your doctor hasn’t approved it, don’t take it.
What Happens If an Interaction Is Found?
Finding an interaction doesn’t mean you have to stop your chemo. It means your care team adjusts your plan. Sometimes, they’ll switch your painkiller from ibuprofen to acetaminophen. Or delay your chemo until you’ve stopped a supplement. Or prescribe a different chemo drug that doesn’t interact with your heart medication. In one case, a woman on tamoxifen for breast cancer was taking an antidepressant called paroxetine. That drug blocked the enzyme needed to turn tamoxifen into its active form. Her cancer risk went up. When her pharmacist flagged it and switched her to a different antidepressant, her treatment worked again. These changes aren’t about fear - they’re about precision. Cancer treatment is no longer one-size-fits-all. It’s about matching the right drug, at the right dose, with the right lifestyle.The Future: Personalized Interaction Risk Scoring
Scientists are now building tools that predict your personal risk of drug interactions based on your genes, age, liver function, and current meds. This is called pharmacogenomics. For example, some people have a gene variant that makes them slow metabolizers of CYP2D6. If they take tamoxifen and a common blocker like fluoxetine, their chemo becomes ineffective. Testing for this gene before starting treatment can prevent treatment failure. Future cancer care will include a “drug interaction score” - like a weather forecast for your treatment. It will tell you: “High risk with this supplement. Avoid. Low risk with this painkiller. Safe.” Right now, that’s still emerging. But the tools are here. The knowledge is growing. And the people who can help you - pharmacists, oncology nurses, care coordinators - are ready.Final Thought: You’re Not Alone in This
It’s easy to feel like you’re managing cancer on your own. But you’re not. There are systems, experts, and protocols designed to catch these dangers before they hurt you. The biggest mistake? Not speaking up. Not asking questions. Thinking that because your oncologist is busy, you shouldn’t bother them with “small stuff.” That supplement you’re taking for your joints? The herbal tea you drink for sleep? The ibuprofen you took for a headache? Those aren’t small. They’re critical. Your treatment is powerful. But it’s also fragile. Protect it - by knowing what’s in your body, asking the right questions, and trusting the experts who’ve seen this before.Can I take over-the-counter painkillers like ibuprofen while on chemotherapy?
It depends. Ibuprofen and other NSAIDs can increase the risk of kidney damage when combined with certain chemotherapy drugs like cisplatin or carboplatin. They can also raise bleeding risk if you’re on blood thinners or taking supplements like fish oil. Acetaminophen (Tylenol) is usually safer, but you should always check with your oncology team before taking any OTC pain reliever.
Is it safe to use CBD oil during chemotherapy?
CBD oil can interfere with the CYP3A4 enzyme system, which many chemotherapy drugs rely on to be broken down. This can cause chemo levels to rise dangerously high, increasing side effects like nausea, fatigue, or low blood counts. There’s not enough research to say CBD is safe with chemo. Most oncologists recommend avoiding it unless part of a monitored clinical trial.
Why can’t I take grapefruit with my chemo?
Grapefruit contains compounds called furanocoumarins that permanently block the CYP3A4 enzyme in your liver and gut. This enzyme breaks down many chemo drugs, including docetaxel, paclitaxel, and etoposide. If it’s blocked, the drug builds up in your blood - which can lead to severe toxicity, organ damage, or even death. One grapefruit can affect you for up to 72 hours. Avoid all forms: juice, fruit, and even flavored products.
Do all supplements interact with chemotherapy?
Not all, but many do. Supplements like St. John’s Wort, garlic, ginger, ginkgo, turmeric, and high-dose vitamins C and E are known to interfere with chemo. Because supplements aren’t regulated like drugs, their ingredients can vary between brands. Even “natural” doesn’t mean safe. Always tell your oncologist about every supplement you take - even if you think it’s harmless.
How do I know if a drug interaction is serious?
Serious interactions can cause sudden symptoms like unexplained bruising or bleeding, severe nausea or vomiting, extreme fatigue, yellowing of the skin or eyes (jaundice), or sudden swelling. If you notice any of these after starting a new medication or supplement, contact your oncology team immediately. Don’t wait. Many serious interactions can be reversed if caught early.
Can my pharmacist help me with chemo interactions?
Yes - and you should ask. Oncology pharmacists specialize in drug interactions and use advanced software to scan your full medication list for risks. They can tell you which supplements to stop, which painkillers are safe, and whether your chemo dose needs adjustment. Most cancer centers have them on staff. Don’t hesitate to request a medication review - it’s a standard part of safe care.
Wayne Keller
Just wanted to say thanks for laying this out so clearly. I’ve been on chemo for 18 months and didn’t realize grapefruit could mess with my meds for days. My wife just threw out our whole citrus basket. Best advice I’ve read all year.
Shana Labed
OMG THIS IS LIFE OR DEATH PEOPLE 😭 I almost took turmeric for my ‘inflammation’ and now I’m sweating just thinking about it. My oncology pharmacist literally screamed at me over the phone when I mentioned it. STOP THE SUPPLEMENTS. YOUR BODY IS A BATTLEFIELD, NOT A YOGA RETREAT.
California Daughter
Wait… so you’re saying I can’t have my ‘immune-boosting’ green juice with ginger, lemon, and turmeric anymore? That’s literally the only thing keeping me sane. Also, who decided grapefruit is evil? It’s a fruit. A beautiful, juicy fruit. This feels like medical overreach.
Vishwajeet Gade
USA medical system is too soft. In India, we just take medicine and shut up. No grapefruit, no supplements, no questions. Chemo is war. You don't argue with your rifle. You take it and survive. Stop overthinking. Just follow doctor.
Casey Crowell
I’m literally crying reading this. 🥹 My mom just got diagnosed and I’ve been Googling everything. This post just saved her life. Thank you. I’m printing this out and handing it to her oncologist tomorrow. Also-pharmacists are unsung heroes. We need more of them. 🙌
Shanna Talley
It’s not about fear. It’s about care. Every pill, every tea, every spoonful of honey-each one is a choice. And choices matter. You’re not alone in this. You’ve got people who see you, not just your diagnosis. Keep asking. Keep sharing. Keep living.
Samuel Wood
Actually, the CYP3A4 mechanism is vastly oversimplified here. Most patients don’t even have the genetic polymorphisms to make this clinically relevant. Also, the 4% mortality stat is from 2001-pre-immunotherapy era. This reads like fearmongering dressed as education. Just sayin’.
ridar aeen
Samuel, you’re missing the point. Even if the stats are outdated, the principle holds: chemo is delicate. Why risk it? The fact that you’re nitpicking the science instead of acknowledging the real-world harm shows how detached you are from patients’ daily reality.
chantall meyer
Most people don’t need this much detail. Just avoid all supplements. Avoid all citrus. Take your pills. Don’t be a hero. Your body isn’t a science experiment. Stop reading blogs and listen to your oncologist.
Lorne Wellington
My cousin just finished treatment and her pharmacist caught a deadly interaction between her chemo and a ‘natural’ sleep aid she’d been using for years. She’s alive today because someone actually checked her list. Seriously-ask your pharmacist. They’re the secret weapon. And yes, that includes your weird herbal tea. 😎
Will RD
Supplements are scams. Grapefruit is fine if you’re not on taxanes. Just stop being paranoid. Your doctor knows what they’re doing. Stop reading Reddit and go take your meds.